
Expired activity
Please go to the PowerPak
homepage and select a course.
INTRODUCTION
Definition and Distinction From Other Forms of Arthritis
Osteoarthritis (OA) is a disease of the entire joint and surrounding tissues.1,2 The term osteoarthritis is derived from three Greek derivations, “osteo,” meaning bone; “arthr,” meaning joint; and “itis," meaning inflammation. One may argue that osteoarthritis is incorrectly named as it is a joint degenerative condition, rather than inflammatory, but this would be a superficial evaluation of a complex, multifactorial condition. It is true that the inflammatory nature of osteoarthritis is not equal to other forms of arthritis such as rheumatoid arthritis (RA); however, chronic low-grade inflammation is very much a component. Synovial tissues from patients with OA exhibit evidence of inflammation, with an infiltration of macrophages and lymphocytes, and inflammation plays a significant role in propagating the joint damage seen in OA.2,3 With a broader appreciation of the involvement of tissues surrounding the articular cartilage, such as the synovium, a better understanding of the complex relationship between mechanical injury/degeneration and inflammatory processes present in OA is becoming elucidated.
EPIDEMIOLOGY
It is estimated that over 32.5 million Americans have OA,4 which is a leading cause of disability and chronic pain.5 The burden placed on individuals with OA is extensive, from physical pain and functional and cognitive impairment to economic hardships seen through increased health care cost and lost income.6 When comparing adults with and without OA in the United States (US), individuals with OA experience a significant increase in pain interfering with daily activities and a significant decrease in function across all functional categories assessed: activities of daily living, physical, social, cognitive, and work.6 OA, although increasing in prevalence with age, is a condition that impacts many age groups and the burden on the quality of one’s life can be detrimental if not properly managed.
Etiology and Pathology
OA is an outcome of an accumulation of risk factors in place of a single etiology.7 Patient factors that may predispose an individual for developing OA may include genetics, but it is unlikely genetics alone will result in the development of OA without the contribution of other factors.7 Leading risk factors for the development of OA include aging, overweight or obese body mass index, genetics, joint overuse, joint trauma, and sedentary lifestyle.1,5,7
The pathology of OA includes cartilage degradation, bone remodeling, formation of osteophytes (abnormal bone growth, also referred to as bone spurs), and synovitis.1 Synovitis (inflammation of the synovium) is now recognized as a key driver in the pathogenesis and severity of OA.2,8 Synovitis presenting in OA is considered “low-grade” in comparison to that presented with RA; however, the extent of inflammation varies.2 Synovial inflammation leads to a decrease in the integrity of protective molecules (hyaluronic acid and lubricin) and an increase in inflammatory molecules such as metalloproteinases and aggrecanases that propagate cartilage degeneration.2 Additional inflammatory components present with OA are the upregulation and activity of inflammatory mediators such as interleukin-1 beta (IL-1β) and tumor necrosis factors (TNF).2,8
Genetics
There are many genes with associated risks for the development of OA, but the overall findings have yet to determine any direct causality.7 Examples of current genetic findings regarding OA risks include polymorphisms of the growth differentiation factor 5 (GDF 5) associated with an increased risk in the development of OA of the hip and knee, and polymorphisms located on the chromosome 7q22 region associated with an increased risk for the development of OA of the knee.7 These are but a few examples, but it is important to explain to patients that regardless of whether they have genetic risks for OA, the severity and outcome of the condition is dependent on many factors that are within their control.
Epigenetics
To further the discussion in support of patient empowerment in the management of their OA, a discussion of epigenetics is needed. Genes are not the sole determinant in how the instructions from one’s genetics will play out. Epigenetics, the study of how behaviors and environment can cause changes that affect the way genes function, has shown that behavioral actions such as exercise and a healthy diet can help to turn “on” and “off” genes in a way that is beneficial to their condition.7,9 Equally so, poor health choices may lead to epigenetic changes that result in expression of genes that are damaging or supportive to the development of OA.7 Epigenetic changes play a critical role in the development of OA.7 Epigenetic mechanisms that can affect gene expression include histone modifications, deoxyribonucleic acid (DNA) methylation, and ribonucleic acid (RNA)-associated silencing.9-11 When a methyl (-CH3) group is added to DNA, it can act as a blockade, inhibiting this gene from being transcribed or “read.”9 Histones are proteins around which DNA is wrapped.9 Modification to this protein can change whether DNA is wrapped around it (turned off) or unwrapped (turned on).9,11 When DNA is unwrapped, it is available to be transcribed, and thus turned “on.”9,11
Diagnosis
It is important for individuals to obtain a formal diagnosis of OA to ensure that an appropriate care plan can be initiated, and to ensure that their joint pain/discomfort is truly as a result of OA in place of other etiologies. The presentation of OA varies depending on the location. However, there are common themes associated with OA, including: morning stiffness (or stiffness following long periods of rest), resolving within 30 minutes of movement; usage-related pain that is relieved with rest; bony enlargement(s) (Heberden’s and Bouchard’s nodes in hand OA); crepitus; and restricted movement (decreased range of motion).12-14
Radiographic evidence is not always necessary for the diagnosis of OA, but it is helpful for monitoring disease progression in hip OA and may be necessary to rule out other etiologies if a patient presents with symptoms not consistent with OA.12 In addition to the symptoms already discussed, symptoms specific to hip OA may include pain in the groin area that radiates into the buttocks region.12 Hand OA also presents with symptoms such as stiffness and swelling, but impairment to use hands for simple tasks such as opening jars and turning doorknobs are the symptoms most problematic for OA in the hands.13
TREATMENT
Pain relief is the primary objective in the management of OA, as it is the existence of pain that results in disability, impaired function, and an overall decrease in the quality of one’s life.6 The American College of Rheumatology (ACR) and the Osteoarthritis Research Society International (OARSI) have provided updated guidelines as of 2019, highlighting new concepts in managing OA with strong emphasis on holistic approaches in managing this multifactorial condition.1,5 It is apparent across both guidelines that there is strong recommendation towards patient education and self-management programs. The consensus and small variations between the nonpharmacologic recommendations are depicted in TABLE 1. Both updated guidelines provide recommendations that are evidenced-based and rich with opportunities for finding nonpharmacologic approaches that are appropriate for the diversity of patients presenting with OA.1,5
| TABLE 1. OARSI vs ACR Nonpharmacological Recommendations1,5 |
| OARSI |
Level of Evidence |
| Type of OA |
Corea |
Level 1Bb |
Level 1Bb |
Level 1Bb |
Level 1Bb |
Level 2c |
Good Clinical Practiced |
| Hip OA |
| No comorbidities |
Arthritis education & structured land-based exercise programs |
Mind-body exercise |
Gait aids |
Self-mgmt programs |
NA |
NA |
Weight mgmt |
| GI comorbidities |
Weight mgmt |
| CV comorbidities |
| Frailty |
NA |
| Widespread pain/depression |
NA |
CBT, self-mgmt. programs |
Pain mgmt program, weight mgmt |
| Knee OA |
| No comorbidities |
Arthritis education & structured land-based exercise programs, mind-body exercise |
Aquatic exercise |
Gait aids |
Self-mgmt programs |
N/A |
CBT with exercise |
N/A |
| GI comorbidities |
| CV comorbidities |
| Frailty |
| Widespread pain/depression |
CBT (w/wo exercise) |
N/A |
Pain mgmt program |
| Polyarticular OA |
| No comorbidities |
Arthritis education & structured land-based exercise programs |
Mind-body exercise |
Dietary weight-mgmt (w/wo exercise) |
Self-mgmt programs |
Gait aids |
N/A |
N/A |
| GI comorbidities |
| CV comorbidities |
| Frailty |
N/A |
| Widespread pain/depression |
Dietary weight-mgmt (w/wo exercise) |
Pain mgmt program |
| ACR |
Strength of Recommendations |
| Type of OA |
Strongly Recommended |
Conditionally Recommended |
| Hand |
Exercise, self-efficacy and self-mgmt programs, first CMC orthosis |
Heat, therapeutic cooling, CBT, acupuncture, kinesiology taping, other hand orthoses, paraffin |
| Knee |
Exercise, self-efficacy and self-management programs, weight loss, tai chi, cane, TF knee brace |
Heat, therapeutic cooling, CBT, acupuncture, kinesiology taping, balance training, PF knee brace, yoga, RFA |
| Hip |
Exercise, self-efficacy and self-mgmt programs, weight-loss, tai chi, cane |
Heat, therapeutic cooling, CBT, acupuncture, balance training |
Abbreviations: ACR, American College of Rheumatology; CBT, cognitive behavioral therapy; CMC, carpometacarpal joint; CV, cardiovascular; GI, gastrointestinal; mgmt, management; N/A, not applicable; OA, osteoarthritis; OARSI, Osteoarthritis Research Society International; PF, patellofemoral; RFA, radiofrequency ablation; TF, tibiofemoral; w/wo, with or without.
aCore: Recommended for all patients with OA as a standard of care.
bLevel 1B: ³75% experts in favor and >50% conditional recommendation.
cLevel 2: 60-74% experts in favor.
dGood Clinical Practice: Supportive information based on expert experience. |
The OARSI guidelines provide guidance with a thorough consideration for comorbidities and medication risks versus benefits.5 Recommendations are organized by OA of the hip, OA of the knee, and polyarticular OA. Additionally, there is focused guidance for each of the following: no comorbidities, gastrointestinal (GI) comorbidity, cardiovascular comorbidity, frailty, and widespread pain/depression.5 The fact that widespread pain/depression is an individual section highlights how important it is to care for this component of the condition, if present. The ACR guidelines are organized by location: hand, knee, and hip.1 Both updated guidelines provide an emphasis on evidenced-based care with a thorough appreciation of the importance of preventive strategies to delay the degeneration of the joint and the corresponding quality of life that follows.
NONPHARMACOLOGIC MANAGEMENT OF OA
Structured Land-Based Exercise Programs
Foundational management for OA, regardless of its location and severity, is arthritis education and structured exercise programs (TABLE 2).1,5 It is advised that regardless of an individual’s comorbidities, pain, disability, or age, exercise is a core component of treatment in OA.1,5,14,15 A national walking program provided by the Osteoarthritis Action Alliance (OAAA) in partnership with the Arthritis Foundation provides a mélange of both education and structured walking programming.16 The initiative, titled “Walk with Ease,” is evidenced-based programming with reported benefits including decreases in pain, improvement in functional ability, and diminished feelings of helplessness regarding ability to manage OA.16
OARSI guidelines have recommended that all OA treatment/management strategies implemented should be on the platform of arthritis education and structured land-based exercises.5 The ACR guidelines strongly recommend self-management and education programs with exercise for all individuals with OA.1 The emphasis on physical activity in OA is based upon exercise providing benefit to all areas of life that may deteriorate in the setting of OA: mental health, physical pain, physical ability, and overall health. Exercise has evidence to minimize pain, improve physical and mental ability, improve mental health, and promote benefit to all areas of one’s health.5,16-20 Prescribed exercise has evidence of improving pain while diminishing the need for pain medication.17,18 Prescribed exercise from a physical therapist and guidance from occupational therapists are highlighted in the ACR guidelines as modalities for individuals to also receive self-management and self-efficacy training, as these are often incorporated.1 Thus, finding the right exercises and receiving guidance and education from physical therapists and occupational therapists are important components of care for all individuals with OA.
Arthritis Education
Arthritis education is now considered a standard of care in the management of OA.1,5 The OARSI guidelines provide the rationale for ongoing arthritis education: “to promote hope, optimism, and a positive expectation of benefit.”5 The psychosocial measures assessed in the Walk with Ease initiative support the importance of achieving these psychological goals; eliminating the feeling of hopelessness to manage OA lends towards better physical health outcomes such as improved function, diminished pain, and overall improvement in the quality of one’s life.16 Education must be ongoing because OA is a chronic condition and management of the disease will change as the condition progresses. Maintaining education helps to better understand the steps that need to be taken respective to where a patient is in their current condition. Life is not static, and neither is anyone’s OA.
Acupuncture
Acupuncture received a conditional recommendation for hand, hip, and knee OA in the ACR guidelines based on the possible benefit and minimal risk of harm.1 The evidence supporting acupuncture in OA is hindered by the difficulty in blinding in studies, and validation of sham versus true acupuncture remains controversial. It is a safe option that may be desirable for those wishing to avoid pharmacological therapy, not attaining sufficient relief from their current regimen, or requiring therapy not associated with drug interactions and medication adverse effects. The most common adverse effect associated with acupuncture is irritation at the site of puncture, but this is generally mild and transient.21
Aquatic Exercise
Aquatic exercise for individuals with OA is evidenced to provide benefit in both pain relief and improvement in function. However, experts recognize that aquatic exercise may not be an accessible option for many. With accessibility and cost providing valid barriers, maintenance may not be likely in large population usage.1,5
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) has to been shown to provide benefit in those with OA, with the most evidence found in those with hip and knee OA, and those with comorbidities of widespread pain and/or depression.5
Mind-Body Exercise
Examples of mind-body exercise are yoga and tai chi. There is growing evidence of the benefit of these types of exercises in OA, as they have been found to be both effective and safe in this setting.5 The research of yoga in OA suggests many beneficial outcomes including a reduction in pain, stress, and depression, while increasing function, sleep, and overall health.22 Tai chi is a combination of slow-flowing postures with deep breathing.22 The benefits obtained through tai chi include mind-relaxation, muscle/ligament stretching, and muscle strengthening.22 Results from a recent study evaluating a dose response of tai chi and physical therapy interventions indicated improvement in pain relief and function directly proportional to the amount of participation in the interventions.19 The more participants attended the classes, the better their scores.19 This highlights the importance of continual activity and the numerous benefits associated with it.
Furthermore, exercise does not have to be hard. It can be enjoyable, and there is exercise appropriate for all levels of fitness. Additionally, when mindfulness exercises are successfully incorporated, there is an increased likelihood of benefit seen from exercise interventions in knee OA.20 Mindfulness-cultivating interventions may therefore further aid in the response obtained from exercise.20 Overall, there is ample opportunity for benefit in patients with OA.
OTC PHARMACOLOGIC MANAGEMENT OF OA
Over-the-counter (OTC) options for OA include acetaminophen, topical capsaicin, and topical (diclofenac) or oral (ibuprofen and naproxen) nonsteroidal anti-inflammatory drugs (NSAIDs). See TABLE 3 for OTC medications and their guideline recommendations in OA management.1,5
| TABLE 3. ACR/OARSI OTC Pharmacology Recommendations1,5 |
| Drugs |
ACR |
OARSI |
| Oral NSAIDs |
Strongly recommendeda,b |
Conditionally recommendeda,b |
| Topical NSAIDs |
Strongly recommendedc |
Strongly recommended |
| Acetaminophen |
Conditionally recommended |
Not recommendede |
| Topical capsaicin |
Conditionally recommendedd |
Not recommendede |
Abbreviations: ACR, American College of Rheumatology; NSAID, nonsteroidal anti-inflammatory drug; OARSI, Osteoarthritis Research Society International.
aRecommended at lowest, effective dose for shortest period of time possible.
bAppropriate for patients without comorbidities, uncertain for patients with moderate comorbidity risk, not appropriate for patients with high comorbidity risk.
cStrong recommendation is for knee OA, with conditional for hand/polyarticular, and no recommendation for hip
dConditionally recommended for knee OA only.
eLack of evidence to recommend. |
Acetaminophen
Acetaminophen was once considered a first-line agent for the use in OA; however, it is becoming increasingly apparent that it is simply not effective, particularly over time.1,5,23 In an analysis comparing treatment options, acetaminophen was found to be the least effective in comparison to oral NSAIDs, topical NSAIDs, and intra-articular therapies (corticosteroids and hyaluronic acids).23 Furthermore, acetaminophen was the only active drug that did not exhibit benefits that were deemed clinically significant.23 The OARSI guidelines conditionally do not recommend acetaminophen in response to the lack of evidence of benefit and growing evidence of hepatotoxicity concerns.5,24 In the setting of OA, acetaminophen may provide the most benefit as an adjunctive agent for pain management, but not as an effective monotherapy option.
OTC formulations of acetaminophen (TABLE 4) include tablets, capsules, liquid, and suppositories, with ranges of regular strength (325 mg), extra-strength (500 mg), and extended-release (650 mg) tablets.25 The 325- to 500-mg tablets may be taken every 4 to 6 hours as needed for pain, while the 650-mg extended-release formulation is designed to be taken every 8 hours.25 The recommended maximum daily dosing of acetaminophen remains at 4000 mg; however, the more conservative recommendation to limit the maximum daily dosing at 3000 mg is prudent for individuals who consume alcohol.25 Ideally, individuals using acetaminophen would avoid alcohol completely, as it increases this risk for hepatoxicity significantly. Hepatotoxicity is a valid concern as acetaminophen remains the leading cause of acute liver failure in the US,24 with 20% of liver transplant cases being attributed to acetaminophen-induced liver failure.26
Capsaicin
Capsaicin is a topical therapy that may be an option for patients not able or wishing to avoid systemic therapy. It acts as a transient receptor potential vanilloid-1 (TRPV1) agonist, stimulating C fibers resulting in an increase of substance P at the initiation of therapy.27-29 Topical capsaicin application will first exhibit a burning sensation in response to the increase in substance P, but over time this sensation diminishes as neural substance P is depleted, resulting in an effective modality for analgesia and desensitization.27-29 There are several benefits seen with capsaicin therapy: 1) it is not systemically absorbed, so it is safe for most patient populations; 2) it may be effective for both musculoskeletal and neuropathic pain relief; and 3) no drug-interactions are known.30
Capsaicin is conditionally recommended in the ACR guidelines for knee OA, while conditionally not recommended for hand OA.1 The biggest concern with the use of capsaicin for hand OA is contamination of the eye.1,29 The OARSI guidelines fail to recommend capsaicin as a result of the poor quality of evidence (TABLE 3).5 However, it is important to note that the highest quality of evidence requires double-blinding in studies, although the localized burning sensation of topical capsaicin inhibits this from being truly possible. As such, it will be difficult to attain this level of evidence. Additional considerations that may not be in favor of topical capsaicin therapy is the burning sensation experienced during the beginning of therapy, the requirement for multiple daily applications in order to attain sufficient benefit, and the level of desensitization and autonomic nerve effects may increase the risk of skin ulcers in patients with diabetes.30,31
The most common adverse effect reported from topical capsaicin therapy is burning at site of application.29 This burning should go away as therapy is continued. Patients should be counseled on the importance of continuous therapy in order to attain the most benefit. This is a chronic therapy that analgesia benefit may diminish if application ceases.29
Topical NSAIDs
Topical NSAIDs are strongly recommended for the use in knee OA, with conditional recommendations for hand OA.1,5 The strength of the recommendation for topical NSAIDs in the setting of hand OA is less than that of knee OA as a result of less randomized-controlled trials evaluating this specific region, rather than concern for harm or lack of efficacy.1,5 Topical NSAIDs attained the strongest recommendation (Level 1A evidence) for use in individuals with knee OA, for those with and without comorbidities as well as those presenting with frailty.5 Topical NSAIDs are the preferred pharmacologic treatment options for knee and hand OA due to the safety profile associated with this delivery formulation, with effective reduction in pain and improvement in function parameters (TABLE 3).1,5,32
The avoidance of systemic exposure results in efficacy at the site of action but circumvents the adverse effects associated with oral NSAIDs (ie, renal, GI, and cardiovascular injury).32 This is extremely important for management in OA as many individuals with OA have GI, cardiovascular, and renal risks that may be mitigated when using topical rather than systemic therapy. In order for a topical NSAID to be effective, it needs to show good penetration of the skin, but not so much that the patient has high systemic exposure. Studies evaluating the systemic exposure of topically applied diclofenac exhibited systemic serum concentrations 0.4% to 2.2% of the concentrations exhibited with orally administered diclofenac.32,33 This provides affirmation of safety of topical application of this drug, while evidence of an adequate amount of diclofenac present in the synovium supports efficacy.33,34
Studies evaluating the efficacy of topical NSAIDs in comparison to oral NSAIDs suggest there is no difference in efficacy, with a statistical difference in favor of topical application in reported adverse effects.32,34 Another benefit recognized with topical NSAIDs is that they have also been found to reduce the need for oral NSAIDs, thus reducing adverse effects and risks associated with oral formulations.32
It is important to note that not all topical NSAIDs are equal in efficacy.31-33 Fortunately, diclofenac, which is highly effective as previously discussed, is now available OTC.34 There is another agent, trolamine salicylate, which is also available OTC, but it has been found to be equal to placebo and is not a topical NSAID that is recommended by the guidelines. When considering an OTC topical NSAID for a patient with OA, only diclofenac should be recommended. The recent change to OTC status of diclofenac permits easy access to a highly evidence-based treatment modality for the management of knee and hand OA. It is not likely to provide benefit with hip OA, as a result of the distance from the joint and the site of application.31-34
Oral NSAIDs
NSAIDs are recommended by the ACR guidelines with the clarification that this recommendation is based on the efficacy of NSAIDs but may not be appropriate in the setting of comorbidities.1 The OARSI guidelines clarify that conditional recommendations for oral NSAIDs are only for individuals with knee OA without comorbidities.5 Oral NSAIDs remain a fairly effective modality for pain relief in the setting of OA; however, they are best reserved for short-term use in light of the risks associated with their use. Oral NSAIDs are associated with GI bleeding/peptic ulcer disease, nephrotoxicity (acute interstitial nephritis, edema, electrolyte imbalance, chronic kidney disease), and cardiovascular risks (hypertension, heart failure, myocardial infarction, stroke).5,35-37 These risks are elevated in the older patient population.36
The guidelines stress the importance of recommending the lowest effective dose for the shortest period of time.1,5 If patients have not received sufficient relief from more conservative therapy and are considering oral NSAID therapy, the lowest formulated dose available OTC is in the combination product with acetaminophen. The ibuprofen dose available in this combination product is 125 mg in place of 200 mg found in single-ingredient ibuprofen formulations.10 TABLE 3 shows the strength of recommendations made for oral NSAIDs in the setting of OA.1,5 TABLE 4 provides a depiction of the different OTC products with dosing recommendations.25,29,30,35,37-39
| Table 4. OTC Medications for OA25,29,30,35,37-39 |
| Drug |
OTC Dosing |
Dosing Adjustments |
Counseling |
Comments |
| Acetaminophen |
325-500 mg 1-2 tab q4-6h NTE 4000/24 h
650 mg ER 1-2 tab q8h NTE 3900 mg/24 h |
Consider lowering total daily dose to 3000 mg if alcohol consumed; risk vs benefit should be evaluated |
Avoid use in hepatic impairment or with alcohol; caution with combination drugs that may also include APAP |
APAP may not be effective as a single agent but may have a place as adjunctive treatment, such as adjunct to topical NSAID or capsaicin |
| Capsaicin |
Topical concentrations: 0.025%, 0.033%, 0.075%, 0.1% |
Consider starting at lowest concentration (0.025%) to work up to higher concentrations in order to diminish discomfort when starting therapy |
Apply tid-qid for max benefit. Interruptions in therapy will result in return to full sensation. Avoid broken skin and mucus membranes. Wash hands diligently following application |
Initiating therapy with once daily dosing may provide necessary accommodation for those more sensitive to the initial burning sensation |
| Diclofenac |
1% topical gel |
N/A |
Use provided dosing card to measure joint-specific dose (2 g for hand, wrist, elbow; 4 g for knee, ankle, foot). Apply up to 4 times daily. Avoid use in patients with aspirin allergy. |
Immediate relief should not be expected; may take a few days to achieve effective pain relief |
| Ibuprofen |
200 mg; 1-2 tab every 4-6 h prn for pain relief. Max of 1200 mg/d for self-treatment, 3200 mg/d under physician’s care |
Consider starting with combination product (APAP/IBU) to minimize NSAID dose; NSAID risks are dose-dependent, so minimizing frequency and dose may prevent harm |
Guidelines recommend the lowest effective dose for the shortest period of time. If GI comorbidities present, consider addition of PPI. Risk vs benefit should be discussed with patient. Avoid use in patients with aspirin allergy |
NSAIDs are listed as possibly inappropriate in the BEERs criteria due to their GI, cardiovascular, and renal risks in the elderly. Avoid in elderly patients with peptic ulcer disease, heart failure, or chronic kidney disease |
Acetaminophen-ibuprofen combination
(APAP 250 mg/IBU 125 mg) |
Take 2 caplets every 8 h prn for pain. NTE 6 cap/24 h |
| Naproxen |
220 mg: 1-2 tab for first dose, followed by only 1 tab every 12 h. NTE 3 tab/24 h |
Start with 1 tab daily. Increase to 1 tab every 12 h if needed. Avoid chronic dosing if possible |
| Abbreviations: APAP, acetaminophen; ER, extended release; GI, gastrointestinal; IBU, ibuprofen; max, maximum; N/A, not applicable; NSAID, nonsteroidal anti-inflammatory drug; NTE, not to exceed; OA, osteoarthritis; OTC, over-the-counter; PPI, proton pump inhibitor; tab, tablet(s). |
For patients with knee OA and GI comorbidities, taking a proton pump inhibitor (PPI) with the NSAID is conditionally recommended to prevent the extent of GI toxicity.1,5 PPIs bring additional risks into consideration, including GI infections (eg, Clostridium difficile), acute kidney injury, and hepatic encephalopathy.40-43 PPI therapy increases gastric pH, which alters intestinal microbial ecology.40 These changes have shown to increase an individual’s risk for C difficile and hospital- and community-acquired pneumonia as well as hepatic encephalopathy.40-43 Additional concern is warranted regarding adverse effects associated with the kidney. PPIs are now a common cause of drug-induced interstitial nephritis with growing evidence supporting their association with chronic kidney disease (CKD) development.41,42 If patients are considering using PPI therapy to mitigate GI toxicity from NSAIDs, the risk associated with PPIs should be considered prior to the initiation of therapy.
PATIENT CASE 1
Beth is a 67-year-old woman who was diagnosed with knee OA several years ago. She began minimizing her activity in response to the discomfort in her knees and now reports that she has gone from being fairly active to leading a sedentary lifestyle. She reports experiencing “creaky, stiff joints” in the morning, but they become less stiff throughout the day. Although they are less stiff as the day progresses, the discomfort she feels does not diminish. She shared with her primary care provider (PCP) that her knees were “continuing to bother her,” and they recommended that she take acetaminophen when she needed relief. Beth explains that she was instructed to take acetaminophen because the other pain medications available were not safe for her since she has high blood pressure (BP) and a family history of heart disease.
Prescription Medication Profile
| Drug |
Dose |
Instructions for Use |
Last Filled Date |
Prescriber |
| Lisinopril/hydrochlorothiazide |
20 mg/12.5 mg |
1 tablet po qd |
11/30/20 |
C. Buffet |
| Rosuvastatin |
10 mg |
1 tablet po qd |
11/30/20 |
C. Buffet |
OTC Supplement Profile
| Drug |
Dose |
Instructions for Use |
| Centrum Silver for Women 50+ |
Multivitamin |
1 tablet qd |
| Glucosamine/chondroitin |
1500 mg/1200 mg |
1 capsule qd |
| Melatonin |
5 mg |
1 tablet qhs |
Objective values: BP 138/88; heart rate 88 beats per minute (bpm); pain scale (1-10): 6.
Social history: Retired librarian, married and lives with spouse. She drinks a glass of wine with dinner each night and does not use any tobacco products.
Family history: She has 2 children and 3 grandchildren. Her father died of a heart attack at the age of 58, and her mother died of complications associated with her diabetes at the age of 65.
PATIENT CASE 2
Bill is a 65-year-old man who has OA in his hands and knees. He is a recently retired architect. Bill’s PCP recommended he initiate topical diclofenac, but he does not like that he has to apply it up to 4 times a day. He would prefer to take something orally, so he does not have to worry about remembering to apply the medication throughout the day.
Prescription Medication Profile
| Drug |
Dose |
Instructions for Use |
Last Filled Date |
Prescriber |
| Atorvastatin |
10 mg |
1 tablet po qd |
11/30/20 |
C. Buffet |
OTC Supplement Profile
| Drug |
Dose |
Instructions for Use |
| Glucosamine/chondroitin |
1500 mg/1200 mg |
1 capsule qd |
Tylenol PM (acetaminophen/
diphenhydramine) |
500 mg/25 mg |
1 tablet qhs |
Objective values: Blood pressure 128/82; heart rate 70 bpm; pain scale (1-10): 5.
Social history: Retired architect, married and lives with spouse. He drinks 1 beer with dinner each night and does not use any tobacco products.
Family history: He has 2 children and 4 grandchildren. Both his parents lived into their 90s. |
MONITORING OTC THERAPIES
Community pharmacists are accessible health care providers that are strategically placed to ensure that safe and appropriate OTC therapy is utilized. One of the key components to safe and effective therapy is ensuring patients are collaborating their care across appropriate disciplines, including their PCPs, physical therapists, and other areas of discipline such as CBT. Of all of the OTC pharmacotherapy options available, monitoring patients utilizing oral NSAIDs is paramount as a result of the risks associated with their use. FIGURE 1 provides a depiction of how the pharmacist can ensure appropriate monitoring and promotion of collaboration in response to monitoring parameters recommended with oral NSAID therapy.37,39,44
| FIGURE 1. Monitoring Parameters for Oral NSAID Therapy Through Pharmacist-Initiated Collaborative Care37,39,44 |
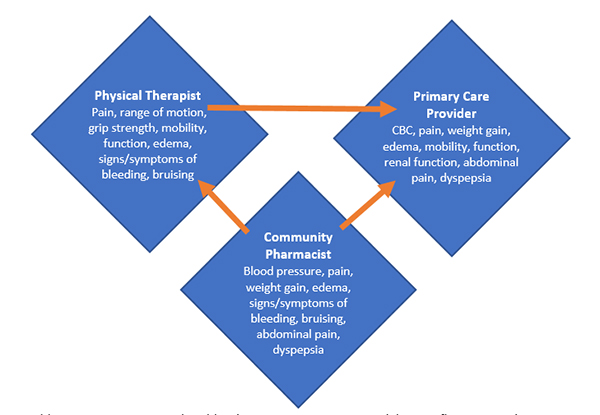 |
| Abbreviations: CBC, complete blood count; NSAID, nonsteroidal anti-inflammatory drug. |
Acetaminophen
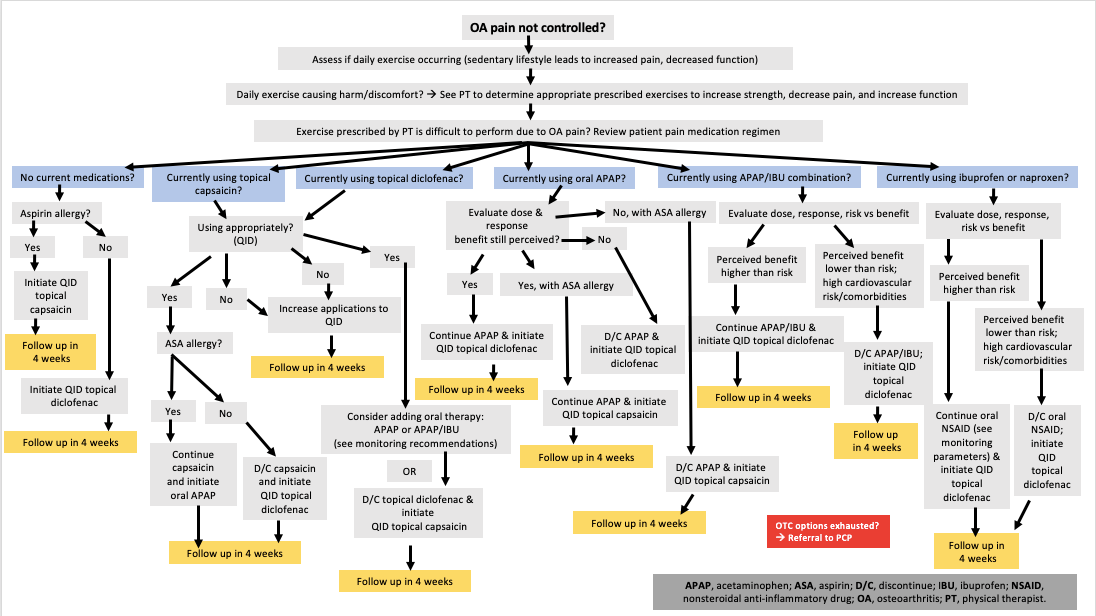
Acetaminophen should be fairly well tolerated but monitoring liver enzymes may be prudent, as hepatoxicity is of growing concern with this treatment modality.24,26 Additionally, counseling about the importance of alcohol avoidance or minimization while taking acetaminophen is another example of something that needs to be evaluated continuously. An important monitoring parameter is ensuring that the patient is attaining appropriate benefit from this therapy. As there is growing concern with the lack of efficacy of acetaminophen in the setting of OA,23 evaluating a patient’s pain and function in response to therapy is important to ensure they do not continue medication beyond the point it provides benefit in place of harm/risk. Refer to FIGURE 2 for OA OTC treatment algorithm recommendations.1,5,25,29,30,34,35,37-39
FIGURE 2. OTC Treatment Algorithm for OA1,5,25,29,30,34,35,37-39 |
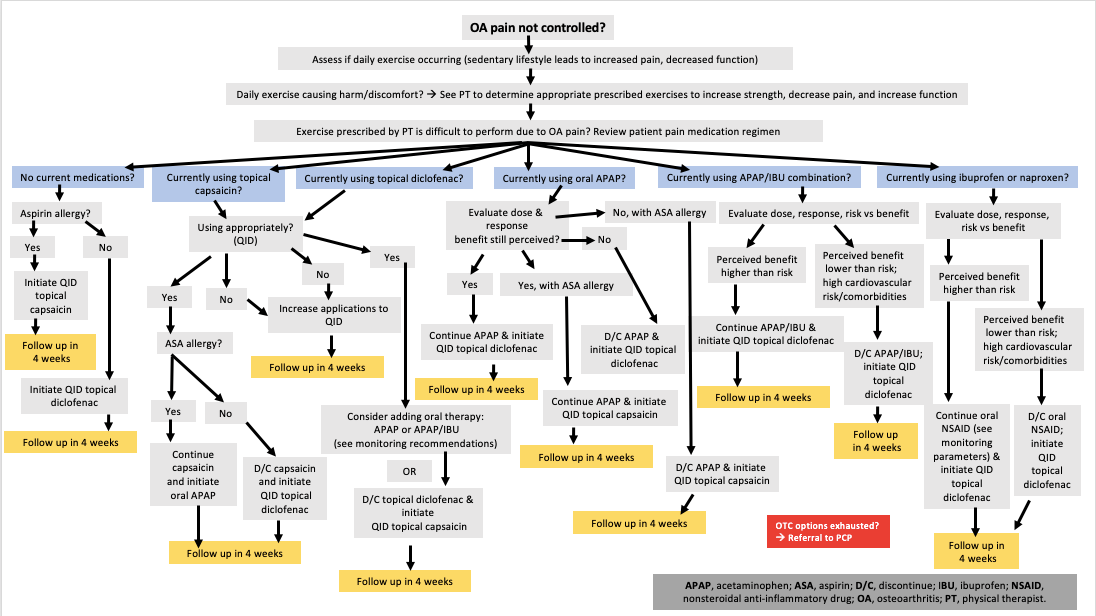 |
Capsaicin
An expected adverse effect of capsaicin is a burning upon application; however, this should diminish over time. If a patient experiences burning that is not tolerable, they should discontinue therapy immediately. Following 3 to 4 weeks of therapy (application to joint 3 to 4 times daily), patients should experience a decrease in pain at the joint in which it is applied and should feel minimal to no burning at the site of application.27,28 Therapy should be continued to maintain benefit.
Diclofenac
Diclofenac is well tolerated, and adverse effects should not be expected. Possible skin irritation may occur, but this should be minimal and go away with time.32-34 Persistent skin irritation would indicate an intolerance to the drug, or some component of the formulation, and application should be discontinued.34
Oral NSAIDs
Oral NSAIDs (ibuprofen and naproxen) are associated with GI, cardiovascular, and kidney injury; thus, monitoring and initiating collaboration with other caregivers is paramount to ensuring patient safety.37,39 Because NSAIDs are readily available OTC, pharmacist-initiated monitoring and collaboration with other health care providers is a key step to preventing adverse events. FIGURE 1 highlights important monitoring parameters that can be performed within each discipline with appropriate overlap in some instances, such as BP and monitoring for weight gain/edema.
PATIENT CASE 3
Emily is a 62-year-old woman experiencing pain and disability as a result of her knee OA. She was diagnosed with knee OA 10 years ago and has been progressively adding more medications to her treatment regimen. At the time of diagnosis, she initiated daily acetaminophen (500 mg, 2 tablets with breakfast and 2 tablets with dinner, if needed). Approximately 2 years following her diagnosis, she increased her daily intake to 1000 mg with breakfast, lunch, and dinner. Her liver enzymes were elevated following an annual visit with her PCP. She was advised to discontinue acetaminophen and initiate topical diclofenac. She responded well to this therapy for several years, but it became evident her OA was progressing as her discomfort level increased and her daily activity decreased. This led to an increase in weight and further decline in her function.
Emily started taking ibuprofen (400 mg with breakfast and dinner) 5 years ago, in addition to her topical diclofenac, and experienced satisfaction with the pain control and resulting daily function. Unfortunately, she was then diagnosed with hypertension and advised to discontinue the ibuprofen. Her PCP also suggested she consider discontinuing her hormone replacement therapy (HRT) in light of her growing cardiovascular risk, but Emily explained that her HRT was not up for discussion and she would not be discontinuing this therapy.
Prescription Medication Profile
| Drug |
Dose |
Instructions for Use |
Last Filled Date |
Prescriber |
| Lisinopril |
20 mg |
1 tablet po qd |
11/30/2020 |
C. Buffet |
| Conjugated estrogens, medroxyprogesterone |
0.3-1.5 mg |
1 tablet po qd |
11/30/2020 |
C. Buffet |
Objective values: BP 130/86; heart rate 86 bpm; pain scale (1-10): 5.
Social history: History professor, divorced and lives alone. She drinks a glass of wine with dinner each night and enjoys a cigar on special occasions.
Family history: She has 1 child (20 years of age). Her father is 88 years old, with no comorbidities, and her mother, 78, has hypertension plus OA of the hip and knees, and myocardial infarction at the age of 70. |
ORAL PRESCRIPTION ANALGESICS
COX-2 Selective NSAID (Celecoxib)
Celecoxib provides another NSAID option that has less GI toxicity than nonselective NSAIDs, but cardiovascular and renal risks remain. Celecoxib has been determined to be noninferior to ibuprofen in knee OA.45
Duloxetine
The serotonin and norepinephrine reuptake inhibitor (SNRI) duloxetine has been approved for the treatment of chronic pain in OA and is conditionally recommended for use in patients with hand, hip, and knee OA.1 The evidence for duloxetine in the setting of OA is based predominately on studies evaluating it for the use in knee OA and for patients with chronic pain.5 It may provide benefit for patients with depression and OA pain; however, evidence is moderate at best. Use with caution in patients with hypertension, as duloxetine may cause or exacerbate hypertension.46 Patients should be counseled that pain relief is not immediate and may take anywhere from 2 to 6 weeks to observe significant improvement in symptoms.46
Opioids
Opioids have fallen out of favor for the use in OA for several reasons. These include: 1) OA is a chronic condition and chronic use of opioids is associated with significant adverse effects in addition to mortality and morbidity risk; 2) over time opioids have shown to have a diminished return in pain relief without a diminishment of adverse effects and harm (ie, constipation, respiratory depression, addiction, death); 3) additional evidence suggests that opioids may result in an increase in pain as a result of a mechanism known as opioid-use hyperalgesia;47 and 4) lastly, a study evaluating the use of opioids prior to knee replacement suggests that opioid use prior to surgery may poorly impact patient outcomes following the surgery.48 Overall, opioids were once considered as an option for those unable to utilize other therapy options, but in the setting of a chronic condition, opioids are not ideal. In the setting in which an individual is unable to use any other medication and is not eligible for surgery, tramadol is recommended in place of other opioids.1
INTRA-ARTICULAR THERAPIES
Intra-articular Corticosteroids
The ACR guidelines strongly recommended intra-articular (IA) corticosteroids for knee and hip OA, with a conditional recommendation for hand OA.1 IA corticosteroids attained a conditional recommendation specific to knee OA, with no recommendation for use in hip or hand OA in the OARSI guidelines.5 Evaluation of the majority of studies investigating this treatment modality in OA suggests that there is modest benefit up to 6 weeks.48 IA corticosteroids have been a long-standing option for short-term pain relief in OA; however, a compelling study by McAlindon et al calls to attention valid concerns with the use of IA corticosteroids in the setting of OA.50 Findings from this trial indicated that 2 years of IA triamcinolone in patients with knee OA resulted in increased cartilage volume loss with no difference from saline injections in pain relief.50 Additional studies have supported these findings and bring rise to the question as to the appropriateness of IA corticosteroids for pain relief in OA.51,52
IA corticosteroids are systemically absorbed and can lead to elevations in BP, blood glucose, salt, and water retention.53,54 In the setting of OA, IA corticosteroids may be an option for short-term pain relief, but long-term efficacy and adverse effects leave this treatment modality as less than ideal.
Intra-articular Hyaluronic Acids
Endogenous hyaluronan is a main component of synovial fluid, providing protective lubricant and viscoelastic properties to the joint.55 Synovial inflammation leads to destruction of this molecule resulting in both a decrease in effectiveness in remaining hyaluronan in the synovium as well as a decrease in the amount of hyaluronan present.55 IA hyaluronic therapy aims to replace this important constituent in the synovial fluid improving elasticity and viscosity in addition to providing anti-inflammatory effects.55,56
A network meta-analysis evaluating the effectiveness of pharmacotherapy options for the treatment of knee OA determined IA hyaluronic acids to be the most efficacious treatment option for pain in comparison to acetaminophen, oral and topical NSAIDs, and IA corticosteroids.23 Additionally, IA hyaluronic acids were found to be statistically superior to IA corticosteroids for the improvement of function.23 IA hyaluronic acids are safe for patients with comorbidities and may prolong the time to which knee replacement is necessary.55 IA hyaluronic acids are generally well tolerated, with injection site irritation and swelling the most common adverse effects reported.55,56
Platelet-Rich Plasma
Platelet-rich plasma (PRP) is a biologic modality that uses a patient’s own plasma to stimulate a healing process at the site of injection.57,58 The exact mechanism of action remains to be determined, however; it is thought that by injecting areas of inflammation with high concentrations of platelets, there may be an acceleration in wound healing.57,58 There is variability in how this procedure is performed as well as variations to the formulation injected into the site of inflammation. In some instances, additional compounds are added to the plasma. As a result of the variability of the process and what is injected, PRP remains to be recommended by any panel of experts until more evidence and consistency is determined.
PHARMACIST ROLE IN OA CARE
Pharmacists are ideally positioned to help individuals with OA navigate treatment options with consideration to comorbidities, concurrent medications, and response to current and/or previous therapies. Pharmacist care in the management of OA has been shown to improve patient utilization of treatments (physical [PT] and pharmacological), decrease pain, increase function, and improve quality of life measures.44 An instrumental role a pharmacist can play for an individual with OA is to recognize when additional or supportive care is needed, such as PT or CBT, and promote the integration of these valuable practices throughout the management of the disease. FIGURE 3 provides a depiction of the integrative care processes that can take place throughout the continuum of OA care.1,5,22,44
| FIGURE 3. Integrative Processes Throughout the Continuum of OA Care1,5,22,44 |
 |
| Abbreviations: CBT, cognitive behavioral therapy; OA, osteoarthritis; PCP, primary care provider; PT, physical therapist; Rx, prescription. |
REFERENCES
- Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Care Res(Hoboken). 2020;72(2):149-162.
- Scanzello CR, Goldring SR. The role of synovitis in osteoarthritis pathogenesis. Bone. 2012;51(2):249-257.
- Rahmati M, Mobasheri A, Mozafari M. Inflammatory mediators in osteoarthritis: a critical review of the state-of-the-art, current prospects, and future challenges. Bone. 2016;85:81-90.
- Centers for Disease Control and Prevention. Osteoarthritis (OA). https://www.cdc.gov/arthritis/basics/osteoarthritis.htm#number. Accessed November 13, 2020.
- Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578-1589.
- Zhao X, Shah D, Gandhi K, et al. Clinical, humanistic, and economic burden of osteoarthritis among noninstitutionalized adults in the United States. Osteoarthritis Cartilage. 2019;27(11):1618-1626.
- Geyer M, Schönfeld C. Novel insights into the pathogenesis of osteoarthritis. Curr Rheumatol Rev. 2018;14(2):98-107.
- Berenbaum F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthritis Cartilage. 2013;21(1):16-21.
- Centers for Disease Control and Prevention. Genomics & precision health. https://www.cdc.gov/genomics/disease/epigenetics.htm. Accessed November 13, 2020.
- Simmons D. Epigenetic influences and disease. Nature Education. 2008;1(1):6.
- Egger G, Liang G, Aparicio A, Jones PA. Epigenetics in human disease and prospects for epigenetic therapy. Nature. 2004;429(6990):457-463.
- Lespasio MJ, Sultan AA, Piuzzi N, et al. Hip osteoarthritis: a primer. Perm J. 2018;22:17-084.
- Kloppenburg M, Kroon FP, Blanco FJ, et al. 2018 update of the EULAR recommendations for the management of hand osteoarthritis. Ann Rheum Dis. 2019;78(1):16-24.
- Zhang W, Doherty M, Peat G, et al. EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis. 2010;69(3):483-489.
- National Clinical Guideline Centre (UK). Osteoarthritis: care and management in adults. London, UK: National Institute for Health and Care Excellence; 2014.
- Osteoarthritis Action Alliance (OAAA). Walk with arthritis (WWE). https://oaaction.unc.edu/resource-library/living-with-osteoarthritis/wwe/. Accessed October 22, 2020.
- Thorlund JB, Roos EM, Goro P, et al. Patients use fewer analgesics following supervised exercise therapy and patient education: an observational study of 16 499 patients with knee or hip osteoarthritis. Br J Sports Med. 2020:bjsports-2019-101265.
- Hammerich AS, Anemaet WK. Applying the evidence for exercise prescription in older adults with knee osteoarthritis. Curr Geri Rep. 2016;5(3):179-190.
- Lee AC, Harvey WF, Price LL, et al. Dose-response effects of tai chi and physical therapy exercise interventions in symptomatic knee osteoarthritis. PM R. 2018;10(7):712-723.
- Lee AC, Harvey WF, Price LL, et al. Mindfulness Is associated with treatment response from nonpharmacologic exercise interventions in knee osteoarthritis. Arch Phys Med Rehabil. 2017;98(11):2265-2273.e1.
- Witt CM, Pach D, Brinkhaus B, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplementmed. 2009;16(2):91-97.
- Arthritis Foundation. Exercises to engage mind and body health. https://www.arthritis.org/health-wellness/healthy-living/physical-activity/yoga/exercises-to-engage-mind-and-body. Accessed October 22, 2020.
- Bannuru RR, Schmid CH, Kent DM, et al. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 2015;162(1):46-54.
- Lancaster EM, Hiatt JR, Zarrinpar A. Acetaminophen hepatotoxicity: an updated review. Arch Toxicol. 2015;89(2):193-199.
- Acetaminophen (OTC). Medscape drug monograph. https://reference.medscape.com/drug/tylenol-acetaminophen-343346. Accessed December 9, 2020.
- Yoon E, Babar A, Choudhary M, et al. Acetaminophen-induced hepatotoxicity: a comprehensive update. J Clin Transl Hepatol. 2016.28;4(2):131-142.
- Caterina MJ, Schumacher MA, Tominaga M, et al. The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature. 1997;389(6653):816-824.
- Nolano M, Simone DA, Wendelschafer-Crabb G, et al. Topical capsaicin in humans: parallel loss of epidermal nerve fibers and pain sensation. Pain. 1999;81(1-2):135-145.
- Groninger H, Schisler RE. Topical capsaicin for neuropathic pain #255. J Palliat Med. 2012;15(8):946-947.
- Guedes V, Castro JP, Brito I. Topical capsaicin for pain in osteoarthritis: a literature review. Reumatol Clin. 2018;14(1):40-45.
- Altman RD, Barthel HR. Topical therapies for osteoarthritis. Drugs. 2011;71(10):1259-1279.
- Rannou F, Pelletier JP, Martel-Pelletier J. Efficacy and safety of topical NSAIDs in the management of osteoarthritis: evidence from real-life setting trials and surveys. Semin Arthritis Rheum. 2016;45(4 suppl):S18-S21.
- McPherson ML, Cimino NM. Topical NSAID formulations. Pain Med. 2013;14(suppl 1):S35-S39.
- Voltaren (diclofenac sodium) topical gel 1% package insert. Warren, NJ: GlaxoSmithKline Consumer Healthcare Inc; 2020.
- Wongrakpanich S, Wongrakpanich A, Melhado K, Rangaswami J. A comprehensive review of non-steroidal anti-inflammatory drug use in the elderly. Aging Dis. 2018;9(1):143-150.
- The 2019 American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694.
- Motrin IB (ibuprofen) package insert. Fort Washington, PA: Johnson & Johnson Consumer Inc; March 2017.
- Advil Dual Action with Acetaminophen (acetaminophen and ibuprofen) package insert. Madison, NJ: Pfizer; 2020.
- Aleve (naproxen) tablets package insert. Whippany, NJ: Bayer; 2020.
- Tantai XX, Yang LB, Wei ZC, et al. Association of proton pump inhibitors with risk of hepatic encephalopathy in advanced liver disease: a meta-analysis. World J Gastroenterol. 2019;25(21):2683-2698.
- Moledina DG, Perazella MA. PPIs and kidney disease: from AIN to CKD. J Nephrol. 2016;29(5):611-616.
- Fossmark R, Martinsen TC, Waldum HL. Adverse effects of proton pump inhibitors¾evidence and plausibility. Int J Mol Sci. 2019;20(20):5203.
- Toda K. Are proton pump inhibitors suitable medicine to prevent gastrointestinal events due to non-steroidal anti-inflammatory drugs? Osteoarthritis Cartilage. 2020;28(1):e1-e2.
- Marra AC, Cibere J, Grubisic M, et al. Pharmacist-initiated intervention trial in osteoarthritis: a multidisciplinary intervention for knee osteoarthritis. Arthritis Care Res (Hoboken). 2012;64(12):1837-1845.
- Gordo AC, Walker C, Armada B, Zhou D. Efficacy of celecoxib versus ibuprofen for the treatment of patients with osteoarthritis of the knee: a randomized double-blind, non-inferiority trial. J Int Med Res. 2017;45(1):59-74.
- Cymbalta (duloxetine) package insert. Indianapolis, IN: Eli Lilly and Company; April 2020.
- Colvin LA, Bull F, Hales TG. Perioperative opioid analgesia-when is enough too much? A review of opioid-induced tolerance and hyperalgesia. Lancet. 2019;393(10180):1558-1568.
- Smith SR, Bido J, Collins JE, et al. Impact of preoperative opioid use on total knee arthroplasty outcomes. J Bone Joint Surg Am. 2017;99(10):803-808.
- Jüni P, Hari R, Rutjes AWS, et al. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev. 2015 Oct 22;(10):CD005328.
- McAlindon TE, LaValley MP, Harvey WF, et al. Effect of intra-articular triamcinolone vs saline on knee cartilage volume and pain in patients with knee osteoarthritis: a randomized clinical trial. JAMA. 2017;317(19):1967-1975.
- Simeone FJ, Vicentini JRT, Bredella MA, et al. Are patients more likely to have hip osteoarthritis progression and femoral head collapse after hip steroid/anesthetic injections? A retrospective observational study. Skeletal Radiol. 2019;48(9):1417-1426.
- Zeng C, Lane NE, Hunter DJ, et al. Intra-articular corticosteroids and the risk of knee osteoarthritis progression: results from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2019;27(6):855-862.
- Yaftali NA, Weber K. Corticosteroids and hyaluronic acid injections. Clin Sports Med. 2019;38(1):1-15.
- Kenalog-40 Injection (triamcinolone acetonide injectable suspension, USP) package insert. Princeton, NJ: Bristol-Myers Squibb Company; 2018.
- Goldwire MA, Shea LA. Intra-articular hyaluronic acids for osteoarthritis of the knee. Drugs Ther Perspect. 2020;36(10):440-450.
- GenVisc 850 (sodium hyaluronate) package insert. Doylestown, PA: OrthogenRx Inc., 2018.
- Raeissadat SA, Rayegani SM, Hassanabadi H, et al. Knee osteoarthritis injection choices: Platelet-rich plasma (PRP) versus hyaluronic acid (a one-year randomize clinical trial). Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1-8.
- Patel S, Dhillon MS, Aggarwal S, et al. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013;41(2):356-364.