
Expired activity
Please go to the PowerPak
homepage and select a course.
Building Pharmacists Skills in Opioid Analgesic Therapy: Defining Pain
Introduction
Pain is a normal physiologic consequence to an injury, or threat of it, that helps protect the body.1 It has been defined as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”2 However, pain can also continue past the point of healing or occur when tissue damage has not occurred.1 Thus, it can be considered a more subjective psychological state as there does not need to be a direct connection between damage and pain.3 Pain is also associated with other comorbidities, and chronic pain can result in numerous health consequences.4 It is estimated that 20.4% of adults in the United States had chronic pain in 2016 and 8% had high-impact chronic pain. Prescription opioids are frequently used to manage pain.5 However, the rise of opioid prescriptions has led to the opioid epidemic. While the number of opioid prescriptions has decreased since 2010 with greater recognition of the potential harms, there continues to be an increase in opioid-related overdose deaths, mainly from illicit opioids.5 In response to the opioid epidemic, the Food and Drug Administration (FDA) supports education for health care providers on appropriate evidence-based principles of acute and chronic pain management.6 A foundational understanding of pain, its pathogenesis, classifications, assessment, and consequences, is essential to assist providers in optimizing pain control and is the subject of this first module for the Opioid Analgesic Therapy Certificate.
Pathogenesis of Pain
Pain results from complex interactions involving both physiological processes and affective or cognitive responses.1,7 Both neural networks and the immune system contribute to the physiological response. Generally, the mechanisms of response to noxious and non-noxious stimuli and involvement of neurotransmitters and neuropeptides are key components of understanding the underlying pathology and rationales for therapeutic options for pain.
Physiologic and pathophysiologic processes
Nociception is the body’s natural process of responding to noxious stimuli.1,7 Nociception involves activation of neural pathways and involves 4 physiological processes: transduction, transmission, modulation, and perception.1 Transduction is initiated by a noxious stimuli, such as trauma, irritation, or extreme temperatures, that activates nociceptors, which are primary afferent neurons.1,7 These neurons activate transduction channels to transmit action potentials. Transmission continues these impulses through the nervous system, namely from peripheral sensory neurons to spinal neurons to the thalamus, which will direct impulses to higher cortical structures in the brain. Modulation is the mechanism where the processing of information can be modified in the brain and spinal cord through neurotransmitters or neuropeptides. This can result in a reduction or enhancement in pain signals. The modulation step is a site of action for many pharmacologic analgesics through influencing neurotransmitters and neuropeptides.7 Finally, perception is the final step where neural activity results in the conscious, subjective experience of pain.1,7 It is thought that this is the site of action of some cognitive approaches to pain management such as relaxation or meditation.7
Pain can also arise in the absence of the noxious stimuli; this maladaptive pain can occur from either peripheral nerve injury or dysfunction or from the central nervous system where there is a disruption in normal pain processing.7 Maladaptive pain is possible due to the plasticity of the nervous system, which allows for changes to occur that result in peripheral or central sensitization.1,7 Central sensitization is a phenomenon where the transmission of pain signals is modulated at the spinal column resulting in amplified transmission (secondary hyperalgesia) or a lowering of the pain threshold to the point where non-noxious stimuli can produce a pain response (allodynia).1,8 Peripheral sensitization occurs when the sensitivity of nociceptors to stimuli increases. Often this occurs due to inflammatory mediators that are present at sites of injury, such as calcitonin gene-related peptide (CGRP) and substance P, which decrease the pain threshold to elicit a response. Thus, a state of primary hyperalgesia or allodynia can occur in response to noxious or innocuous stimuli, respectively. Further, sensitization can excite nociceptors resulting in ectopic discharges causing spontaneous pain. Lastly, pain signals can also be modified at the supraspinal level.1 Descending pain modulation describes pathways that originate from the brain down to the spinal cord resulting in modification of incoming somatosensory information to change the perception and reaction to stimuli, which can result in an increase or decrease in pain.
Neurochemistry
While changes in pain systems can occur at an anatomic level, an understanding of the neurochemistry involved in modulating pain is likely most informative for pharmacists.8,9 Numerous neurotransmitters are involved in pain transduction and transmission, and in the descending pain modulation pathways. These neurotransmitters act as mediators, interact with channel-linked receptors, and impact pre- and post-synaptic neurons. A discussion of all these mechanisms involved in the pain process is beyond the scope of this review; however, a few are worth highlighting here. For more in-depth information, the reader is directed to a freely available article on this topic that can be accessed here.10
The major excitatory neurotransmitters involved in the somatosensory system are glutamate and aspartate.9,10 They are found broadly in both the central and peripheral nervous systems at synapses. Both interact with several receptors, which include the N-methyl-d-aspartate (NMDA) receptor, a target for some pharmacologic therapies for pain. In contrast, the major inhibitory neurotransmitters are glycine and gamma-aminobutyric acid (GABA). Glycine is located at the spinal level, whereas GABA is located higher up in the central nervous system and at presynaptic terminals. The role of agonists and antagonists of GABA in pain is complex and seemingly paradoxical. For example, low doses of GABAA agonists (eg, muscimol) at primary afferents can reduce pain, whereas higher doses can potentiate pain.9 Additionally, in animals models, GABA antagonists (eg, bicuculline) have decreased hypersensitivity through action at the dorsal root ganglion. Development of pharmacologic therapies that selectively and specifically take advantage of GABA receptors has not been hugely successful; however, certain medications, such as benzodiazepines, are thought to exert some of their effects through modulation of the GABAA receptor.
Neuropeptides also contribute to somatosensory signaling in the pain system.9,10 In contrast to neurotransmitters, neuropeptide actions are more likely to have a gradual onset and a prolonged duration, unlike the rapid onset and offset of neurotransmitters. Excitatory neuropeptides include substance P and CGRP. Substance P’s activation of neurokinin receptors is considered a key mechanism in the induction of sensitization and subsequent hyperalgesia.9 Inhibitory neuropeptides include opioid peptides and cannabinoids. The opioid peptide receptors, mu-, kappa-, and delta-subtypes, are widely distributed throughout the nervous system and are targets for prescription opioid therapies.
Types of Pain
Multiple classifications exist that categorize pain.7,11 Most commonly, pain is subdivided by its duration, intensity, and type or underlying pathophysiology. While not discussed below, other characterizations specific to disease states where pain is a prominent symptom are also available (eg, fibromyalgia, cancer pain).3
Classification by duration
Pain can be subdivided by duration into acute and chronic, with acute pain typically lasting less than 30 days, while chronic pain lasts longer than 3 or 6 months.7 Acute and chronic pain differ in many other ways as well. In general, acute pain results from the normal physiological response to noxious stimuli. This response is an adaptive process that works as a warning system to help avoid potentially harmful situations. However, acute pain can still result in deleterious effects, particularly if it is severe in intensity or undertreated. In contrast, chronic pain can be present in the absence of noxious stimuli or injury. The underlying etiology may not be obvious or identifiable and be a consequence of abnormal nerve function or transmission. With its chronic nature, additional psychological and quality of life impact can occur. Table 1 provides an overview of keys differences between acute and chronic pain.
| Table 1. Comparison of Characteristics Between Acute and Chronic Pain.7,12 |
| Characteristic |
Acute pain |
Chronic pain |
| Pathophysiology |
Typically results from noxious stimuli |
Organic cause may be absent |
| Typical sources |
Results from injury, tissue damage, or inflammatory processes |
Results from chronic disease or untreated conditions |
| Duration |
Limited – can resolve over days to weeks, typically associated with healing |
Can begin gradually, but persists over time from months to years |
| Psychological component |
May have anxiety or restlessness
Depression and insomnia less common |
Commonly associated with depression, fatigue, and insomnia |
| Environmental/family issues |
Generally minor |
Can impact quality of life including increased financial burden and increased dependence on family and the health care system |
| Dependence/tolerance to medication |
Unusual |
Common |
| Treatment goal |
Cure |
Improved functionality |
Classification by intensity
While the experience of pain is subjective, the intensity of pain is an important component of characterization.13 There are many scales available to assess intensity, which are described more fully later in this module, but generally pain can be described as mild, moderate, or severe. Assessment of pain intensity is also critical to determine if treatments are providing clinically meaningful relief. For example, on a 0 to 10 numerical rating scale (NRS), reductions of 10% to 20%, ≥ 30%, and > 50% represent minimally important, moderately important, and substantial improvement in pain, respectively.
Classification by pathophysiology
Pain can also be subdivided based on its underlying pathophysiology.14 There are 3 key types to consider:
- Nociceptive: Occurs in response to noxious stimuli. Considered to be part of the normal, adaptive consequence of pain
- Inflammatory: Occurs after tissue damage or infection that results in an increased sensory sensitivity. Considered to be part of the normal, adaptive consequence of pain by minimizing the body’s physical contact and movement.
- Maladaptive: Occurs when there is a disruption or abnormal functioning of the normal pain pathway. Can occur if there is damage to the nervous system (neuropathic pain) or in the absence of any injury or inflammation (dysfunctional pain).
There are some differences in the nomenclature for these categories and most attention in the literature focuses on differences in nociceptive and neuropathic pain. Nociceptive pain can further be categorized into somatic and visceral pain.8,12 Key characteristics between these pain types are summarized in Table 2.
| Table 2. Comparison of Characteristics of Nociceptive and Neuropathic Pain.8,12 |
| Characteristic |
Nociceptive Pain |
Neuropathic Pain |
| Cause |
Damage to tissue; can be superficial (somatic pain) or deep (visceral pain) |
Injury to peripheral or central nervous system that results in maladaptive changes |
| Example sources of pain |
Postoperative pain, infection, osteoarthritis, lower back pain, pancreatitis, organ metastasis |
Nerve compression, phantom limb pain, diabetic neuropathy, chemotherapy-induced neuropathy, radiculopathies |
| Example pain descriptors |
Sharp, burning, throbbing, aching, cramping, stabbing |
Shooting, electric-like, stabbing, burning, tingling, painful numbness |
| Sensory effects |
Generally absent |
Common; manifests as numbing, tingling |
| Hypersensitivity |
If present, localized to area of injury |
More likely to be present; could manifest as hyperalgesia or allodynia |
| Autonomic symptoms |
Generally absent |
Up to a third of patients may experience temperature changes, swelling, or sweating |
Pain Assessment and Screening
With pain being a subjective experience, self-reporting is needed in pain assessment.13,15 There are several evidence-based, standardized scales or tools that can be used. Acute pain is generally easier and more reliably assessed as one-dimensional tools evaluating intensity can be used. However, chronic pain with its multidimensional nature can become more complex as functional ability, affective components, and quality of life may also need to be measured. Additionally, characterization of location, pain descriptors (eg, aching, shooting), and functional aspects (ie, occurring at rest vs during activities) should be included in a pain history.13 Lastly, it should be noted that additional instruments are available beyond those discussed below, including ones better targeted for the pediatric population. For example, the Wong-Baker FACES pain rating scale does not require language, which is useful for younger children or those who have barriers in communicating verbally.15
Standardized instruments for pain intensity
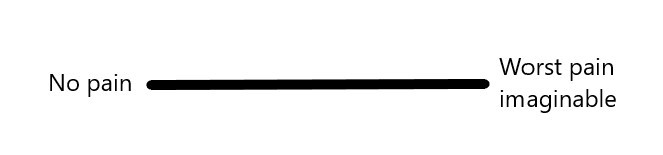
While there are many validated scales available, the 3 most commonly used scales for measuring pain intensity are the verbal rating scale (VRS), NRS, and visual analog scale (VAS).13,15 Each of these one-dimensional instruments asks patients to self-report their pain by having them rate it along an ordinal scale. For VRS, descriptive categories are provided in an ordered set allowing a patient to select the descriptor that best fits their pain (eg, “none” to “very severe”). The NRS uses numerals with verbal anchors to provide a scale (eg, 0 [no pain] to 10 [most intense pain imaginable]). The VAS uses a line with verbal anchors on each end and patients are instructed to place a mark at the point that their pain intensity falls (Figure 1). Some research indicates that the VAS may be the most preferred tool of the 3 options based on its sensitivity, but the NRS might be more practical and easier to use as it does not require physical presence, clear vision, or dexterity to complete.
Figure 1. Example of a visual analog scale (VAS) – often 10 cm long and scored using a ruler.
Standardized instruments for multidimensional assessment
There are several instruments available for practice and use in clinical trials, but the McGill Pain Questionnaire (MPQ) and its short-form version (SF-MPQ) are used widely. 15,16 The MPQ is a multidimensional tool that evaluates different components of the pain experience and is validated in multiple populations including those with chronic pain. Three dimensions are evaluated, which include sensory-discriminative, affective-motivational, and cognitive-evaluative.15 The instrument includes 20 sets of verbal descriptors that are used to evaluate sensory (10 sets), affective (5 sets), evaluative (1 set), and miscellaneous (4 sets) components of pain. Patients select the words that best describe their pain and these results are converted and assigned a value for scoring. The SF-MPQ is a more contemporary tool and consists of 15 items of verbal descriptors, which are divided into sensory (11 items) and affective (4 items). Each descriptor is ranked on an ordinal intensity scale from 0 (none) to 3 (severe). A revision was published in 2009 for a second short form version, SF-MPQ-2, which can be used in neuropathic and non-neuropathic pain conditions.17 This version amended the SF-MPQ to include 7 additional items related to neuropathic pain, for a total of 22 items with 0 to 10 numerical response options. The descriptors fall along 4 subscales, which include continuous pain descriptors (6 items; eg, “throbbing pain”), intermittent pain descriptors (6 items; eg, “shooting pain”), predominately neuropathic pain descriptors (6 items; eg, “hot-burning pain”), and affective descriptors (4 items; eg, “tiring-exhausting”).
Standardized instruments for neuropathic pain
For neuropathic pain conditions, there is growing research into screening and assessment questionnaires.18,19 Screening questionnaires are geared toward assisting in the diagnosis of neuropathic conditions by differentiating symptoms from other types of pain. Some examples include the Douleur Neuropathique 4 (DN4), Leeds Assessment of Neuropathic Symptoms and Signs, and PainDETECT, which can all be used as rapid screening tools by non-pain specialists. Assessment questionnaires can be used to evaluate the pain itself and to monitor treatment outcomes for neuropathic symptoms. Along with the more general SF-MPQ-2, the Neuropathic Pain Scale and the Neuropathic Pain Symptom Inventory are a couple examples of assessment questionnaires; additionally, there are some data to support use of the PainDETECT instrument for assessment.
Standardized instruments for evaluating other domains
Both functional status and quality of life are additional domains that also can be assessed.20 In fact, the Centers for Disease Control and Prevention (CDC) recommend assessment of function and quality of life in addition to pain intensity in patients with chronic pain. The instrument recommended by the CDC for functional assessment is the Pain, Enjoyment of life, General Activity (PEG) tool, which assesses both pain intensity and interference with daily living. It is a 3-item scale that includes an NRS and asks how pain has interfered with enjoyment of life, as well as general activity.21 Other functional assessments are available, but in general these are less well-validated instruments and some that are available were created for specific populations, such as the Roland-Morris Disability Questionnaire for back pain.22 Health-related quality of life and daily activity disruption may be assessed with other instruments. A few examples include Patient-Reported Outcomes Measurement Information System (PROMIS; a general tool for measuring symptoms, function, and quality of life in chronic disease) and the Pain Disability Index (a pain-specific tool for measuring the degree of interference to daily life). For a more in-depth review, the reader is directed to a review article by Turk and colleagues that provides a good summary of available instruments for the assessment of psychosocial and functional aspects of chronic pain.22
Screening tools for opioid addiction or abuse
It may also be helpful to identify and manage risk prior to initiating opioid therapy by screening patients who may be at increased risk for opioid use disorder, addiction, or abuse.7,23 There are several risk factors thought to increase the risk for opioid prescription abuse; one single risk factor is not likely to be determinate, but an assessment of multiple factors is needed to predict this risk. Some risk factors include sociodemographic factors, pain and drug-related factors, genetics, and psychosocial history. The most predictive risk factor for opioid misuse is a history of substance use disorder, which includes illicit drugs, tobacco, and alcohol. Several opioid-specific screening tools are available for screening and monitoring of abuse, though none is widely accepted as a gold standard.24,25 A couple of examples of instruments that can be used for screening prior to starting chronic opioid therapy include the Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R) and the Opioid Risk Tool. The latter tool can be completed in about 1 minute, which may be valuable in settings where time is more limited.25
Consequences of Undertreated Pain
Development of chronic pain
One undesirable consequence of undertreated acute pain is potential conversion to a chronic pain state.26,27 Typically, short-term pain causes changes to neuronal receptors, ion channels, and proteins along with the release of pro-inflammatory mediators to the area of injury.26 Persistent pain may remodel the nervous system to cause sensitization and amplify the body’s response to pain. Higher intensity and longer duration of pain increase the risk for developing chronic pain.26-28
Some patients are at a higher risk for developing chronic pain compared to others. Between 10% to 60% of patients with improperly treated post-surgical acute pain develop chronic pain.27,29-31 Besides higher intensity and longer duration of pain, other risk factors predisposing patients to chronic pain include younger age, female sex, obesity, smoking, genetic predisposition, and previous pain experiences.27 Psychological factors - anxiety or depression before a procedure, pessimistic or catastrophizing tendencies, and/or fear of pain - affect perception and resolution of pain, which may contribute to the development of chronic pain.27,29
Proper prevention and management of pain with analgesia may prevent acute pain from turning into chronic pain.28,29 Reducing the intensity of acute pain and employing less invasive surgical procedures, which causes less damage to major nerves, are also effective approaches.29
Physical impacts
Undertreated pain limits physical function and contributes to the physical deterioration of patients.32,33 Pain intensity, duration, and location can influence the level of physical function.32 For example, pain can reduce mobility in the lower extremities resulting in difficulties with standing up, walking, and/or climbing stairs. 32,33 Patients with pain, especially older adults, experience slower gait speeds, impaired gait function, decreased walking distance, and reduced ability to exercise.33 Undertreated multisite pain affecting the upper extremities impairs the patient’s ability to reach overhead, to grip, and to carry items weighing as little as 10 pounds. Patients with fibromyalgia or generalized pain typically have difficulties in getting up or sitting down.32
Undertreated pain has substantial consequences on quality of life; it is well-documented that stronger intensity, higher frequency, and chronic pain leads to a lower quality of life.26,28,32 Sleep disturbances, which increase stress levels and impair cognitive abilities, are common among patients with pain.26,32 Pain intensity and sleep disturbances exhibit bidirectional effects, where a night of poor sleep increases pain intensity the next day, and vice versa.34 Chronic pain impairs sexual function by causing difficulties with arousal, confidence, performance, and relationships, and by patients fearing worsening pain.26 Older adults with multisite pain display poor balance and coordination, increasing the risk of falls.33 Falls may lead to severe outcomes such as disability, hospitalization, and even death in this patient population. Undertreated pain can limit the ability to perform activities of daily living and increase the risk of disability.28,33 Patients with pain struggle with completing domestic chores and participating in social activities.26,32 Close to 50% of patients report that pain prevents them from participating in social or family activities.35 For example, patients with neuropathic pain hesitate to plan social activities due to the unpredictable nature of pain.32
Pain does not only affect patients but also their family members and caretakers.32 Because patients may experience disability due to pain, family members play a more active role in taking care of these patients. Family members may become primary caretakers, make decisions regarding treatments, and supervise these treatments. The new responsibilities may cause feelings of sadness, overburden, overwhelming state, and frustration and may affect their daily, professional, and social lives. Many primary caretakers develop anxiety and depression and sometimes experience greater discomfort than patients themselves. These experiences can affect the family unit and cause relationship difficulties between patients, caregivers, and their partners.
Psychological impacts
Patients with undertreated pain experience several mental and psychological consequences. Studies have shown that depression affects 5% to 100% of people with chronic pain.22,33 Depressive symptoms are especially common among women with pain and contribute to pain-related disability. Negative thoughts associated with depression further prolong the pain experience.22 Anxiety, described as feelings of worry and nervousness about future issues, affects around 35% of patients with chronic pain.22,36 Panic and post-traumatic stress disorders are up to 3 times more likely to be present among patients with chronic pain compared with the general population.36 Feelings of fear, defined as worry and nervousness emotions about the present state (ie, desire to escape or avoid something in the present), and pain avoidance exacerbate the pain experience.22 Specifically, fear and pain avoidance cause dysfunctional cognitive processes, contributing to psychological disability and potentially leading to impaired physical function. Patients with chronic pain experience memory and attention difficulties due to physical changes within the brain.26 Other potential psychological consequences of chronic pain include suicidal ideation and attempts.
Catastrophizing, one of the maladaptive behaviors to undertreated pain, further worsens the pain experience.22 Patients who catastrophize, which involves assuming the worst outcomes for even minor issues, display negative perceptions, expectations, and memories that worsen the pain experience. Rumination, helplessness, increased attention to pain, and negative anticipation of pain are common behaviors among patients with catastrophizing tendencies. Catastrophizing may lead to onset of pain, increased postoperative pain severity, transition from acute to chronic pain, and pain-related disability. Catastrophizing affects patients not only on the psychological level but also on the physiological level. In patients with moderate pain, catastrophizing decreases the activity of the descending pain modulation inhibitory system making the disengagement from pain more challenging. In patients with mild pain, catastrophizing mainly affects the brain regions responsible for attention, vigilance, and emotion, translating into increased attention and negative anticipation of pain.
Psychological consequences of undertreated pain lead to a myriad of other negative consequences. Feelings of helplessness and lower self-efficacy contribute to higher pain intensity, poor physical and psychological adjustment to pain, and disability.22 Self-efficacy is defined as a personal conviction to reach the desired outcome in a specific situation. Lower self-efficacy may lead to impaired physical function and work absenteeism. Additionally, negative psychological experiences may contribute to fewer years of education, and as a result, lower income.33
Economic impacts
Undertreated or improperly treated pain increases the economic burden for both the patient and the health care system and can lead to its overuse.32 Up to 70% of patients with chronic pain visit primary care providers, and the average number of medical visits can reach 9 within 6 months.32,37 Uncontrolled post-procedural pain is responsible for up to one-third of unanticipated readmissions.38 The risk factors for an increased number of visits or readmissions consist of higher pain intensity and longer duration, poor health, comorbidities, and psychological issues (eg, depressive symptoms).32,39,40
Undertreated pain impacts the economic situation of individual patients as well. Work absenteeism, job loss, voluntary resignation, early retirement, and switching to a more accommodating or work-from-home job are potential consequences that face patients with pain.32,37 Among patients remaining in the workforce, productivity declines as pain intensity increases.32 Such changes in employment or productivity affect the economic stability of patients and may even contribute to the loss of needed health benefits.
Conclusion
Overall, there are many complexities and factors that contribute to pain and its modulation. While there is biologic value to pain as an adaptive survival mechanism, the physiology, neurochemistry, and mediators of pain can shift to a maladaptive role, leading to chronic pain. Pain can be classified by its duration, intensity, and type of underlying pathophysiology. An understanding of the type of pain is an important component of pain management as it directs treatment options, as improperly treated or undertreated pain can lead to many physical, psychosocial, and economic consequences. Several evidence-based, standardized scales or tools are available to assess patients with pain that differ in their purpose and dimensionality in assessing different components of the pain experience.
A summary of key terminology from this section is presented in Table 3.
| Table 3. Key Terminology.8,14 |
| Terminology |
Definition |
| Allodynia |
Pain that occurs in response to an innocuous stimulus (does not normally cause pain) |
| Descending modulation |
Modification of incoming somatosensory input through pathways that descend from the brain to the spinal cord that alter perception of and reactions to stimuli leading to increased or decreased pain |
| Dysfunctional pain |
Pain that occurs in the absence of any injury or inflammation |
| Hyperalgesia |
Increased pain that occurs in response to a stimulus that does normally cause pain |
| Inflammatory pain |
Pain that occurs after tissue damage or infection that results in an increased sensory sensitivity |
| Neuropathic pain |
Pain that results from a lesion or disease of the somatosensory system |
| Nociception |
The process of encoding noxious stimuli |
| Nociceptive pain |
Pain that results from actual or threatened damage to the body that activates nociceptors |
| Noxious stimulus |
A stimulus that is damaging or threatens damage to normal tissues |
| Sensitization |
Increased responsiveness of nociceptive neurons to their normal input and/or recruitment of a response to normally subthreshold inputs; can occur centrally or peripherally |
References
- Ringkamp M, Dougherty PM, Raja SN. Anatomy and physiology of the pain signaling process. In: Benzon HT, Raja SN, Liu SS, et al, eds. Essentials of Pain Medicine. 4th ed. Philadelphia, PA: Elsevier; 2018. https://www.clinicalkey.com/#!/browse/book/3-s2.0-C20140038373. Accessed April 10, 2020.
- Bonica JJ. The need of a taxonomy. 1979;6(3):247-248.
- Merskey H. Taxonomy and classification of chronic pain syndromes. In: Benzon HT, Rathmell JP, Wu CL, et al, eds. Practical Management of Pain. 5th Philadelphia, PA: Elsevier; 2014. https://www.clinicalkey.com/#!/browse/book/3-s2.0-C20090640630. Accessed April 10, 2020.
- Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of chronic pain and high-impact chronic pain among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(36):1001-1006.
- Guy GP, Jr., Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697-704.
- FDA education blueprint for health care providers involved in the treatment and monitoring of patients with pain. Food and Drug Administration website. Updated September 2018. https://www.fda.gov/media/99496/download. Accessed April 10, 2020.
- Herndon CM, Ray JB, Kominek CM. Pain management. In: DiPiro JT, Yee GC, Posey L, et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 11th New York, NY: McGraw-Hill; 2019. http://accesspharmacy.mhmedical.com/content.aspx?bookid=2577§ionid=226724502. Accessed April 10, 2020.
- Cohen SP, Mao J. Neuropathic pain: mechanisms and their clinical implications. 2014;348:f7656.
- Nouri KH, Osuagqu U, Boyette-Davis J, et al. Neurochemistry of somatosensory and pain processing. In: Benzon HT, Raja SN, Liu SS, eds. Essentials of Pain Medicine. 4th Philadelphia, PA: Elsevier; 2018. https://www.clinicalkey.com/#!/browse/book/3-s2.0-C20140038373. Accessed April 10, 2020.
- Yam MF, Loh YC, Tan CS, et al. General pathways of pain sensation and the major neurotransmitters involved in pain regulation. Int J Mol Sci. 2018;19(8). doi: 10.3390/ijms19082164.
- Rathmell JP, Fields HL. Pain: pathophysiology and management. In: Jameson J, Fauci AS, Kasper DL, et al, eds. Harrison's Principles of Internal Medicine. 20th New York, NY: McGraw-Hill; 2018. http://accessmedicine.mhmedical.com/content.aspx?bookid=2129§ionid=192010846. Accessed April 10, 2020.
- Ellison DL. Physiology of pain. Crit Care Nurs Clin North Am. 2017;29(4):397-406.
- Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth. 2008;101(1):17-24.
- Woolf CJ. What is this thing called pain? J Clin Invest. 2010;120(11):3742-3744.
- Lazaridou A, Elbaridi N, Edwards RR, et al. Pain assessment. In: Benzon HT, Raja SN, Liu SS, et al, eds. Essentials of Pain Medicine. 4th ed. Philadelphia, PA: Elsevier; 2018. . Accessed March 19, 2020.
- Main CJ. Pain assessment in context: a state of the science review of the McGill pain questionnaire 40 years on. 2016;157(7):1387-1399.
- Dworkin RH, Turk DC, Revicki DA, et al. Development and initial validation of an expanded and revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2). 2009;144(1-2):35-42.
- Attal N, Bouhassira D, Baron R. Diagnosis and assessment of neuropathic pain through questionnaires. Lancet Neurol. 2018;17(5):456-466.
- Morgan KJ, Anghelescu DL. A review of adult and pediatric neuropathic pain assessment tools. Clin J Pain. 2017;33(9):844-852.
- Implementing the CDC guideline for prescribing opioids for chronic pain. Centers for Disease Control and Prevention website. Published 2018. https://www.cdc.gov/drugoverdose/pdf/prescribing/CDC-DUIP-QualityImprovementAndCareCoordination-508.pdf. Accessed April 10, 2020.
- Krebs EE, Lorenz KA, Bair MJ, et al. Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. J Gen Intern Med. 2009;24(6):733-738.
- Turk DC, Fillingim RB, Ohrbach R, et al. Assessment of psychosocial and functional impact of chronic pain. J Pain. 2016;17(9 Suppl):T21-49.
- Kaye AD, Jones MR, Kaye AM, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 1. Pain Physician. 2017;20(2s):S93-S109.
- Kaye AD, Jones MR, Kaye AM, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 2. Pain Physician. 2017;20(2s):S111-S133.
- Assessment tools. Washington State Agency Medical Directors' Group website. http://www.agencymeddirectors.wa.gov/AssessmentTools.asp. Accessed April 10, 2020.
- Fine PG. Long-term consequences of chronic pain: mounting evidence for pain as a neurological disease and parallels with other chronic disease states. Pain Med. 2011;12(7):996-1004.
- Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287-2298.
- Sinatra R. Causes and consequences of inadequate management of acute pain. Pain Med. 2010;11(12):1859-1871.
- Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. 2006;367(9522):1618-1625.
- Poobalan AS, Bruce J, Smith WC, et al. A review of chronic pain after inguinal herniorrhaphy. Clin J Pain. 2003;19(1):48-54.
- Johansen A, Romundstad L, Nielsen CS, et al. Persistent postsurgical pain in a general population: prevalence and predictors in the Tromso study. 2012;153(7):1390-1396.
- Duenas M, Ojeda B, Salazar A, et al. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457-467.
- Butera KA, Roff SR, Buford TW, et al. The impact of multisite pain on functional outcomes in older adults: biopsychosocial considerations. J Pain Res. 2019;12:1115-1125.
- O'Brien EM, Waxenberg LB, Atchison JW, et al. Intraindividual variability in daily sleep and pain ratings among chronic pain patients: bidirectional association and the role of negative mood. Clin J Pain. 2011;27(5):425-433.
- Moulin DE, Clark AJ, Speechley M, et al. Chronic pain in Canada--prevalence, treatment, impact and the role of opioid analgesia. Pain Res Manag. 2002;7(4):179-184.
- McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. 2003;106(1-2):127-133.
- Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287-333.
- Coley KC, Williams BA, DaPos SV, et al. Retrospective evaluation of unanticipated admissions and readmissions after same day surgery and associated costs. J Clin Anesth. 2002;14(5):349-353.
- Azevedo LF, Costa-Pereira A, Mendonca L, et al. Chronic pain and health services utilization: is there overuse of diagnostic tests and inequalities in nonpharmacologic treatment methods utilization? Med Care. 2013;51(10):859-869.
- Von Korff M, Lin EH, Fenton JJ, et al. Frequency and priority of pain patients' health care use. Clin J Pain. 2007;23(5):400-408
Back to Top