
Expired activity
Please go to the PowerPak
homepage and select a course.
Primer on Prevention and Treatment of HIV Infection
INTRODUCTION
Human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) continue to plague patients worldwide despite remarkable advances in antiretroviral therapies. This is best exemplified by the 2015 “Indiana outbreak” in Scott County, Indiana, which garnered national attention after HIV incidence increased significantly over a short period of time.1 The Scott County outbreak, which was fueled by injection drug abuse, shows that issues beyond access to care are perpetuating HIV infection in the United States.
The purpose of this activity is to provide an update on nonpharmacologic and pharmacologic interventions for HIV infection and review testing-related requirements of the Florida Omnibus AIDS Act.
EPIDEMIOLOGY
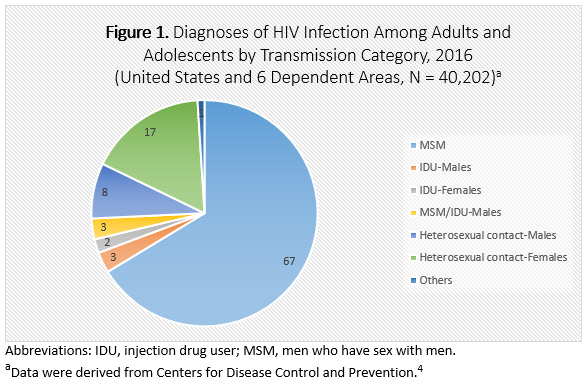
In 2017, approximately 37 million people were living with HIV infection worldwide.2 Interestingly, the global incidence decreased from 2010 to 2017 by an estimated 16%, which is thought to be related to reductions in heterosexual transmission.2,3 In the United States, an estimated 39,782 people were newly diagnosed with HIV infection in 2016; the number of new infections decreased by 8% compared with 2010–15.4 Despite efforts to test, treat, and retain patients in care, select populations in the United States continue to be disproportionally affected, especially African Americans and men who have sex with men (MSM).4 Figure 1 illustrates the percentage of HIV infection diagnoses in 2016 among adolescent and adult Americans by method of transmission.
New diagnoses of HIV infection appear to be concentrated in the southeastern United States. Data from one epidemiologic study showed that more than one-half of all newly diagnosed patients are from the South,5 which may be the result of a complex interplay between demographic, economic, and social networks.6,7 Furthermore, 3 of the top 5 states in terms of HIV infection (rates per 100,000 population) are located in the southeastern United States4: District of Columbia, 55.6; Georgia, 31.8; Louisiana 29.7; Florida, 28.1 and Maryland, 21.7.
The continued burden on those affected by HIV infection was the impetus for the National HIV/AIDS strategy to close the chasm between patients who are diagnosed or are unaware of their HIV status and virologic suppression. The burden also continues to be recognized globally and has resulted in the ambitious “90-90-90 target”: 90% of patients knowing their HIV status, 90% of those with an HIV diagnosis being on active therapy, and 90% of those on therapy achieving virologic suppression.8
OVERVIEW OF HIV INFECTION
HIV infection cannot be fully eradicated from the body. Consequently, available treatments focus on slowing viral replication, which occurs rapidly in gut-associated lymphoid tissue and the central nervous system.9,10 The primary target of HIV infection is the CD4 T-lymphocyte (CD4 cell). Multiple co-receptors facilitate HIV entry into CD4 cells, and these have become pharmacologic targets in recent years: C-C chemokine receptor type 5 (CCR5) and C-X-C chemokine receptor 4 (CXCR4).3 Viral replication within human CD4 cells eventually leads to immune suppression, which increases the body’s susceptibility to a number of opportunistic infections.
Acute HIV infection usually displays high viral replication in conjunction with a decline in CD4 cells 1 to 4 weeks after exposure. Unfortunately, the clinical presentation of HIV infection is similar to nonspecific viral illnesses such as mononucleosis and influenza, making diagnosis of acute infection difficult.11 Common symptoms include fever, lymphadenopathy, and maculopapular rash. Further, HIV antibodies are usually not identifiable until 4 to 6 weeks postinfection. This delayed production in HIV antibodies is known as the “window period.” As a result, diagnostic tests often do not have the capability to detect infection during this timeframe, which can result in a false-negative test result (a result that appears negative when it should not).
After acute HIV infection, patients may enter a latent stage during which HIV ribonucleic acid (RNA) remains relatively stable and CD4 cells are gradually depleted. However, as HIV infection progresses and a patient’s immune system becomes increasingly compromised, the transition to AIDS eventually occurs. A diagnosis of AIDS is made when a patient’s clinical condition meets any one of the following criteria12:
- Laboratory confirmation of HIV infection and CD4 count less than 200 cells/mm3
- Laboratory confirmation of HIV infection and CD4 percentage less than 14%
- Laboratory confirmation of HIV infection and any AIDS-defining condition (Table 1)
| Table 1. AIDS-Defining Conditions |
Candidiasis of bronchi, trachea, or lungs
Candidiasis of esophagus
Cervical cancer, invasive
Coccidioidomycosis, disseminated or extrapulmonary
Cryptococcosis, extrapulmonary
Cryptosporidiosis, chronic intestinal (>1 month's duration)
Cytomegalovirus disease (other than liver, spleen, or nodes), onset at age >1 month
Cytomegalovirus retinitis (with loss of vision)
Encephalopathy, HIV-related
Herpes simplex: chronic ulcers (>1 month's duration) or bronchitis, pneumonitis, or esophagitis (onset at age >1 month)
Histoplasmosis, disseminated or extrapulmonary
Isosporiasis, chronic intestinal (>1 month's duration)
Kaposi sarcoma
Lymphoid interstitial pneumonia or pulmonary lymphoid hyperplasia complex
Lymphoma, Burkitt
Lymphoma, immunoblastic
Lymphoma, primary, of brain
Mycobacterium avium complex or Mycobacterium kansasii
Mycobacterium tuberculosis of any site, pulmonary, disseminated, or extrapulmonary
Mycobacterium, other species or unidentified species, disseminated or extrapulmonary
Pneumocystisjirovecii pneumonia
Pneumonia, recurrent
Progressive multifocal leukoencephalopathy
Salmonella septicemia, recurrent
Toxoplasmosis of brain, onset at age >1 month
Wasting syndrome attributed to HIV
Source: Reference 13 |
In clinical practice, patients frequently present with advanced disease because they are unaware of their HIV status. This reinforces the importance of closing the gap between identifying individuals who are unknowingly infected and treating them with the most appropriate therapies.
TRANSMISSION OF HIV
HIV infection can be transmitted through sexual contact, injection drug use (IDU), contact with certain body fluids, vertical transmission (mother-to-child transmission) and, to a lesser extent, exposure to blood products.14 Because of consistent screening practices that are in place for blood donors and blood products, transmission via this route has become exceedingly rare.15 Body fluids that are recognized to pose a high transmission risk include semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, peritoneal fluid, pericardial fluid, and amniotic fluid. HIV infection is not thought to spread via air or water; casual contact, such as washing dishes or shaking hands; insects; or toilet seats.16
When assessing the risk of HIV acquisition, receipt of infectious blood products and IDU carry the highest risk. In contrast, sexual acquisition depends on HIV RNA plasma levels of the infected patient, number of encounters with an infected partner, and type of sexual contact. Receptive anal sex carries a higher risk of acquisition than penile vaginal intercourse.14
Infection Control Practices in the Health Care Setting
From an infection control perspective, percutaneous needlesticks and exposure to body fluids are primary risk factors for HIV transmission. Data presented at the 2015 Conference on Retroviruses and Opportunistic Infections (CROI) indicated the last case of nosocomial transmission occurred in 1999, which serves as a testament to the effectiveness of universal precautions and postexposure prophylaxis.17 The purpose of Occupational Safety and Health Administration (OSHA) universal workplace precautions is to prevent parenteral, mucous membrane, and nonintact skin exposures to blood-borne pathogens. These precautionary measures include the following18:
- Using appropriate barriers such as a gown, gloves, and eye protection
- Safely handling and disposing of needles and other sharps
- Immediately washing skin surfaces after contact with blood or body fluids
The risk of acquiring a blood-borne pathogen through a needlestick injury is quantifiable in what is commonly referred to as the Rule of 3s19:
- For hepatitis B virus (HBV) the risk is 30%
- For hepatitis C virus (HCV) the risk is 3%
- For HIV infection the risk is 0.3%
In the event that an occupational exposure does occur, health care workers should wash wounds and skin sites with soap and water, flush mucous membranes with water, and determine the HIV status of the source patient when possible.19 Notably, multiple state laws indicate that a patient must understand and agree to HIV testing (i.e., informed consent), which means the patient (not the health care provider) determines if testing may take place.20 Procedures related to informed consent in Florida are discussed later in this manuscript.
Methods of Prevention of Transmission
The primary modes of HIV transmission are sexual intercourse, percutaneous injury, and IDU. However, over the past several decades, a more detailed understanding of HIV transmission has led to the development of various preventive measures, including safer sex practices, needle exchange programs, and preexposure prophylaxis (PrEP) and postexposure prophylaxis (PEP).
Safer sex practices
Concerning safer sex practices, the following patient recommendations may help reduce the risk of HIV transmission18:
- Limiting the number of sexual partners: Having multiple partners increases the chances of coming into contact with someone whose viral load is not suppressed or someone who has a sexually transmitted disease (STD).
- Choosing low-risk sexual behaviors: Anal receptive sex is the highest-risk sexual activity followed by vaginal and oral sex, respectively.
- Using condoms: Female condoms are just as effective as male condoms at preventing HIV and STDs. For male condoms, latex products provide the best defense against HIV infection because natural membrane condoms (lambskin) are porous, which limits their ability to protect against HIV and STDs. Importantly, even though male and female condoms are highly effective at reducing HIV transmission, neither is completely effective.
- Getting tested: For people who are sexually active, annual testing for STDs is recommended, considering these infections can increase the likelihood of transmitting HIV or acquiring it from others.
- Remaining adherent to treatment: For people who are HIV positive, it is important that they start and stay on antiretroviral treatment because these strategies have shown to greatly reduce the possibility of transmitting HIV infection to others.
Injection drug use
For those individuals who use injectable drugs, the best method to reduce HIV transmission is abstinence. However, some individuals may find it difficult to stop or refuse to seek help. In these circumstances, the following interventions should be recommended by health care practitioners, which may help reduce HIV transmission18,21:
- Use only new, sterile needles, syringes, and other injection equipment—and never share.
- Clean used needles and syringes with bleach only when new ones are not available, which may reduce the risk of transmitting or acquiring HIV. Notably, the following document from the Centers for Disease Control and Prevention (CDC) website provides more detailed information about syringe disinfection practices for individuals who are unable to stop using drugs: http://www.cdc.gov/idu/facts/disinfection.pdf
- Dispose of needles and syringes safely through the use of a sharps container and keep used needles and syringes away from other people.
- Encourage patients to discuss PrEP and nonoccupational PEP with health care practitioners. Each of these interventions is discussed below.
Pre-exposure prophylaxis
The United States Public Health Service (USPHS) guidelines recommend evaluating male and female patients whose sexual or injection drug behaviors place them at high risk of acquiring HIV infection.22 While efforts are ongoing to diagnose and treat patients, clinics in the United States have emphasized PrEP to prevent new infections in high-risk seronegative patients or serodiscordant couples.
The only PrEP medication regimen approved by the Food and Drug Administration (FDA) is tenofovir disoproxil fumarate/emtricitabine (Truvada), a fixed-dose combination tabletadministered once daily or in an “on-demand” dosing strategy.23 It is important to note that tenofovir disoproxil fumarate and emtricitabine are available as individual agents; however, they should not be used as PrEP individually. All patients who receive PrEP should be evaluated according to the timeframes listed below to determine the overall safety and effectiveness of tenofovir disoproxil fumarate/emtricitabine and to assess for signs and symptoms of HIV infection (Table 2).22
| Table 2. Recommended Monitoring for Pre-exposure Prophylaxis |
At least every 3 months:
- Repeat HIV testing and assess for signs or symptoms of acute infection
- Repeat pregnancy testing for women who may become pregnant
- Provide a prescription or authorize refills of tenofovir disoproxil fumarate/emtricitabine
- Assess treatment adherence and side effects related to tenofovir disoproxil fumarate/emtricitabine
- Provide ongoing support for risk-reduction behaviors
At least every 6 months:
- Ensure tenofovir disoproxil fumarate/emtricitabine is not causing renal damage and assess for additional side effects
- Conduct recommended testing for sexually transmitted infections
At least every 12 months:
- Evaluate the need to continue PrEP as a preventive measure
Source: Reference 22
Abbreviation: Preexposure prophylaxis, PrEP |
Clinical studies have validated PrEP's overall efficacy. One of the first studies to demonstrate benefit, the Chemoprophylaxis for HIV Prevention in Men (iPrEx) Study, evaluated a daily tenofovir disoproxil fumarate/emtricitabine regimen compared with placebo in a MSM patient population.24 PrEP reduced risk of HIV acquisition by an average of 44% among patients randomized to receive active drug. Despite these findings, providers continue to be hesitant to prescribe pre-exposure drug regimens because of concerns related to cost, fostering antiretroviral resistance, drug toxicity, and behavioral risk compensation (adjustment of individual behavior in response to perceived changes in risk; people tend to behave more cautiously if their perception of risk or danger increases, and less cautiously when they feel protected). Studies to date have not substantiated any of these concerns.25,26
Postexposure prophylaxis
Postexposure prophylaxis involves an individual taking 3 or more antiretroviral medications as soon as possible after he or she has been exposed to potentially HIV-infected material. PEP interventions are indicated after 2 types of exposures: occupational PEP and nonoccupational PEP.14,19
- Occupational PEP (oPEP) interventions are administered when an individual is exposed to a potential source of HIV in the workplace (e.g., hospital setting).
- Nonoccupational PEP(nPEP) interventions are administered when a potential HIV exposure occurs outside the workplace (e.g., IDU, sexual assault, unprotected sex).
Multiple government agencies collaborated in 2011 to form the USPHS Working Group for the purpose of updating the 2005 Guidelines for the Management of Occupational Exposures to HIV and Recommendations for Postexposure Prophylaxis. The updated guidelines indicate oPEP regimens should contain at least 3 antiretroviral drugs for all occupational exposures, and the regimen should be continued for 28 days.19 Specifically, tenofovir disoproxil fumarate/emtricitabine plus raltegravir is considered first-line therapy because this combination is tolerable, potent, convenient, and is associated with limited drug interactions. Alternative oPEP drug regimens can be found by accessing the updated USPHS guidelines at the following CDC website: http://stacks.cdc.gov/view/cdc/20711. Notably, the drugs listed below are not recommended to be included in PEP regimens for the following reasons19:
- Nevirapine is contraindicated because of serious toxicities related to liver and muscle damage.
- Abacavir should only be used under the direction of expert consultation because of the need to identify individuals who are at high risk for hypersensitivity reactions (those who carry the HLA-B*5701 allele).
- Enfuvirtide is not recommended because it requires subcutaneous administration.
- Efavirenz should not be used during the first trimester of pregnancy or for women who may become pregnant while taking PEP due to risk of teratogenicity.
Clinical guidance for nPEP is offered through multiple organizations, including CDC, Health Resources and Services Administration (HRSA) HIV/AIDS Bureau, and the New York State Department of Health AIDS Institute.19,27,28 Patients who may have been exposed to HIV infection and are considered to be high risk should commence a 3-drug antiretroviral combination immediately, and the regimen should be continued for 28 days. The Medical Care Committee at the New York State Department of Health and HRSA HIV/AIDS Bureau now recommend tenofovir disoproxil fumarate/emtricitabine plus raltegravir or dolutegravir as the preferred initial nPEP regimen.27,28
For individuals who may have been exposed to a source of HIV-infected material, successive HIV testing and laboratory panels are necessary to rule out infection and assess drug toxicity (when therapy is recommended). Suggested patient follow-up is typically included in health care facility protocols, or recommendations can be found in oPEP and nPEP guidelines. Health care professionals may also contact a PEP hotline for guidance through the CDC and University of California at San Francisco at (888) 448-4911. Moreover, when either type of exposure occurs, pharmacists and other health care professionals should at a minimum provide the following patient education14,27:
- Educate high-risk individuals regarding the availability of PrEP and nPEP.
- Advise patients to begin PEP regimens as soon as possible (when a drug regimen is indicated). Data suggest uncertainty regarding clinical benefit/protection if the regimen is not commenced within 72 hours of exposure.
- Educate patients about the efficacy of PEP, timely initiation of the medications, adherence to the regimen for 28 days, and the importance of preventing additional HIV exposures during this time.
- Counsel patients about the importance of committing to serial HIV and laboratory testing to minimize drug toxicity and to rule out HIV infection. Re-evaluation of patients who have been exposed should begin within 72 hours after the initial exposure.
- Instruct patients to contact their health care provider immediately if they experience uncomfortable adverse effects after commencing a PEP drug regimen. An alternative regimen may be needed to lessen adverse effects and improve adherence.
- Advise patients who have been exposed to use latex barriers with their sex partners until transmission of HIV infection has been ruled out.
- Counsel patients about the symptoms of HIV infection and instruct them to contact their medical provider immediately if these develop.
- Refer sexual assault victims to a qualified health care professional who can provide a baseline evaluation and appropriate counseling.
DIAGNOSTIC TESTS
While antiretroviral therapy has been revolutionized, so has the ability to test and diagnose patients with HIV infection. Available HIV tests include enzyme-linked immunosorbent assays (ELISA), Western blot, HIV RNA, and rapid HIV tests. Two rapid HIV tests, OraQuick In-Home HIV Test and the Home Access HIV-1 System, are both FDA-approved over-the-counter in-home test kits.
OraQuick In-Home HIV Test provides results in approximately 20 minutes and requires only an oral swab. Studies have shown Oraquick has an expected performance of approximately 92% for test sensitivity (i.e., the percentage of results that will be positive when HIV is present) and an expected performance of 99.9% for test specificity (i.e., the percentage of results that will be negative when HIV is not present).29 The rapid availability of a test result makes OraQuick appealing to patients. However, the speed at which a test result is produced must be carefully weighed against false negatives that may occur during the “window period” as well as the need for subsequent evaluation based on the initial test result. Accordingly, pharmacists have the opportunity to play an integral role in providing guidance to patients regarding testing.
The Home Access HIV-1 System is also available over the counter. Notably, this system requires a blood sample that must be shipped to a laboratory for testing. Patients are able to call approximately 1 week later with a code specific to their kit to receive their test results. Studies have shown the sensitivity and specificity of the Home Access HIV-1 System to be greater than 99.9%.30
The Western blot has been the confirmatory assessment after a positive result from an ELISA test. However, the Western blot has been supplanted by HIV-1/2 differentiation immunoassay because the latter provides earlier identification of positive test results.31
INITIATION OF ANTIRETROVIRAL THERAPY—MEDICATION ADHERENCE AND DRUG INTERACTIONS
Treatment options and health care services for patients with HIV infection have advanced significantly since the virus was discovered in the 1980s. Clinicians are able to select antiretrovirals from 6 different drug classes in order to construct an ideal patient-specific drug regimen. However, numerous factors should be considered before making therapeutic decisions. These factors are highlighted in Table 3.
| Table 3. Factors to Consider When Selecting Antiretroviral Therapy |
| Age/gender |
Cost |
| Adherence to current medications |
HLA-B*5701 results |
| Occupation |
Genotypic results |
| Comorbidities |
Tolerability and adverse effect profile |
| Child-bearing age and family planning |
Pill burden and frequency of dosing |
| Access to care |
Drug interactions and pharmacokinetic profile |
| Concomitant medications |
Pretreatment viral load/CD4 count |
| Source: Reference 12, 32 |
Perhaps 2 of the most important factors that must be taken into consideration before initiating antiretroviral medications are the patient’s willingness to adhere to a prescribed drug regimen and drug-drug interactions. Several strategies to improve adherence and retention in care include12:
- Assessing the patient’s knowledge of HIV infection
- Providing each patient with necessary HIV-related resources
- Recognizing the patient’s readiness to start antiretroviral therapy
- Identifying barriers or reasons for nonadherence at baseline and with every clinic visit
- Involving the patient in antiretroviral drug selection
- Using treatment adherence interventions such as mobile applications (apps)
- Systematically monitoring patients to retain in care
Drug-drug interactions must be considered as well. Notably, certain antiretroviral drug classes have shown a greater propensity for clinically relevant interactions because of their pharmacokinetic (PK) profiles. PK interactions may occur during oral absorption, metabolism, or elimination of an antiretroviral or the interacting drug. Three common mechanisms that influence the oral absorption of select antiretrovirals include: elevated gastrointestinal (GI) pH, cationic chelation, and changes to p-glycoprotein function.12 Many patients who are on antiretroviral medications take antacids, histamine-2 blockers (H2 blockers), or proton pump inhibitors (PPIs). Consequently, systemic concentrations of atazanavir and rilpivirine, among others, are reduced because each of these agents requires an acidic gastric medium for oral absorption.12 The bioavailability of rilpivirine is affected significantly with concomitant PPI use and therefore is contraindicated. For patients taking atazanavir who require stomach acid–reducing drugs, counseling patients to take antiretrovirals 2 hours after antacid therapy or 12 hours after an H2 blocker or PPI may help mitigate concerns regarding drug-drug interactions.12
Two major enzyme systems play a significant role in drug-drug interactions: cytochrome P-450 (CYP450) enzymes and uridine diphosphate (UDP)-glucuronosyltransferase (UGT) 1A1. The CYP450 enzyme system influences the metabolic breakdown of many antiretrovirals, including nonnucleoside reverse transcriptase inhibitors (NNRTI), protease inhibitors (PI), and entry inhibitors. Protease inhibitor–based regimens are particularly challenging because they are coadministered with ritonavir or cobicistat (pharmacoenhancers). The purpose of a pharmacoenhancer is to increase or “boost” the concentration of an antiretroviral medication. However, because numerous medications share metabolic pathways, the “boosting” effect of pharmacoenhancers frequently leads to various CYP-mediated interactions. In addition, the coadministration of pharmacoenhancers with systemic and local corticosteroids can result in adrenal insufficiency and Cushing’s syndrome. As a result, corticosteroids are not recommended to be coadministered with “boosted” antiretroviral regimens unless the potential benefits outweigh the risks. Notably, data suggest beclomethasone may be the safest treatment option when an inhaled corticosteroid must be coadministered with a “boosted” antiretroviral drug regimen.12
The UDP-UGT 1A1 enzyme system is primarily responsible for the metabolism of integrase inhibitors, including bictegravir, dolutegravir, and raltegravir. Consequently, each of these medications is mostly devoid of CYP-mediation drug interactions, but they may be involved in other clinically relevant drug interactions. For a comprehensive list of CYP450-mediated drug interactions involving antiretrovirals and commonly used acute and chronic medications, the following link to the Department of Health and Human Services (DHHS) HIV guidelines is recommended12: https://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescent-arv/0
Antiretroviral Medications
HIV treatment guidelines were revised significantly in 2015 with continual changes made annually.12 Efavirenz is no longer recommended as a preferred treatment option because of its central nervous system-related adverse effects, which negatively impacted patient tolerability. Both darunavir and atazanavir each boosted with ritonavir or cobicistat are now considered alternative regimens, based largely on outcomes from the AIDS Clinical Trials Group (ACTG) A5257 study.33 Similar to efavirenz, the efficacy of atazanavir is limited by patient tolerability attributed to its adverse effects. While integrase strand transfer inhibitors (INSTIs) are now considered preferred treatment options because of improved patient tolerability and overall drug efficacy, the DHHS guidelines current as of October 2018 relegated the elvitegravir-containing regimen to second-line because of its propensity for drug-drug interactions.12
For both treatment-experienced and treatment-naive patients, antiretroviral therapy is recommended to reduce the risk of disease progression as well as prevent the transmission of HIV infection. The most recent iteration of the guidelines recommends all patients be started on antiretroviral therapy regardless of current CD4 count. This recommendation is based on the findings of the Strategic Timing of Antiretroviral Treatment (START) study.34 When constructing an antiretroviral drug regimen for any patient, 3 or more fully active agents should be included. For treatment-naïve patients, it is universally recommended to include 2 nucleoside reverse transcriptase inhibitors (NRTIs) in combination with a third active drug from the integrase inhibitor class. It is important to note that while both tenofovir formulations are approved by FDA, tenofovir alafenamide has fewer toxicities and has largely replaced tenofovir disoproxil fumarate in most settings. Tables 4 through 9 detail available antiretroviral treatment options, including adult dosing and clinical pearls about each therapy. Currently recommended drug regimens for treatment-naive patients according to updated HIV guidelines include the following12:
- Abacavir/lamivudine/dolutegravir onlyfor patients who are HLA-B*5701 negative
- Tenofovir/emtricitabine plus dolutegravir
- Tenofovir/emtricitabine plus raltegravir
- Tenofovir/emtricitabine/bictegravir
Table 4. Entry (Fusion) Inhibitors |
Generic Name
(Brand Name) |
Route of
Administration |
Clinical Pearls |
Usual Adult Dosing |
Enfuvirtide
(Fuzeon) |
Subcutaneous |
- Requires reconstitution for subcutaneous administration
- Associated with an increased risk of bacterial pneumonia
- FDA approved for treatment-experienced patients only
|
90 mg (1 mL) twice daily |
Maraviroc
(Selzentry) |
Oral |
- Black-box warning for hepatotoxicity
- Only active against CCR5-dominant virus
|
150 mg to 600 mg twice daily |
Ibalizumab-uiyk
(Trogarzo) |
Intravenous |
- FDA approved in combination with other antiretrovirals in heavily treatment-experienced patients with multidrug-resistant virus failing their current antiretroviral regimen
|
2000 mg as a single dose followed by a maintenance dose of 800 mg every 14 days |
| Source: Reference 12 |
| Abbreviations: CCR5, C-C chemokine receptor type 5. |
| Table 5. Nucleoside/Nucleotide Reverse Transcriptase Inhibitors |
Generic Name
(Brand Name) |
Route of
Administration |
Clinical Pearls |
Usual Adult Dosing |
Abacavir
(Ziagen) |
Oral |
- Requires HLA-B*5701 testing to assess risk for hypersensitivity
- Associated with risk of myocardial infarction
- Only NRTI that does not require dose adjustment for renal dysfunction
|
600 mg once daily
300 mg twice daily |
Didanosine
(Videx EC) |
Oral |
- Take on an empty stomach
- Pancreatitis; peripheral neuropathy
- Not commonly used due to toxicity profile
|
<60 kg: 250 mg once daily
≥60 kg: 400 mg once daily |
Emtricitabine
(Emtriva) |
Oral |
- Minimal side effects
- Active against HBV; avoid abrupt discontinuation in co-infected patients
|
200 mg once daily |
Lamivudine
(Epivir) |
Oral |
- Minimal adverse effects
- Active against HBV; avoid abrupt discontinuation in co-infected patients
|
300 mg once daily
150 mg twice daily |
Stavudine
(Zerit) |
Oral |
- Pancreatitis; peripheral neuropathy
- Not commonly used due to toxicity profile
|
<60 kg: 30 mg twice daily
≥60 kg: 40 mg twice daily |
Tenofovir disoproxil fumarate
(Viread) |
Oral |
- Take with food
- Integral part of NRTI drug regimens
- Active against HBV
|
300 mg once daily |
Tenofovir
alafenamide/emtricitabine
(Descovy*) |
Oral |
- Considered to be the replacement for tenofovir disoproxil fumarate in NRTI backbones
- Significantly diminished toxicities due to lower systemic concentrations
|
25/200 mg once daily |
Zidovudine
(Retrovir) |
Oral and
intravenous |
- Bone marrow suppression; malaise
- Clinical utility in reducing perinatal HIV transmission specifically in intrapartum care
|
300 mg twice daily |
| Source: References 12, 35, 36 |
| Abbreviations: HBV, hepatitis B virus; NRTI, nucleoside reverse transcriptase inhibitor. *Available as a coformulated tablet with emtricitabine (Descovy) for HIV infections and as a single-ingredient tablet formulation for infections of hepatitis B virus (Vemlidy). |
| Table 6. Nonnucleoside Reverse Transcriptase Inhibitors |
Generic Name
(Brand Name) |
Route of Administration |
Clinical Pearls |
Usual Adult Dosing |
Delavirdine
(Rescriptor) |
Oral |
- Avoid antacids
- Not commonly used due to high pill burden and lower efficacy
|
400 mg three times daily |
Doravirine
(Pifeltro) |
Oral |
- Lacks central nervous system adverse effects
- Not affected by acid-suppressive agents
|
100 mg once daily |
Efavirenz
(Sustiva) |
Oral |
- Take at bedtime on an empty stomach to limit central nervous system adverse effects
- Consider avoiding in patients with coexisting psychiatric disorders
- Associated with increased risk of self-harm
|
600 mg once daily |
Etravirine
(Intelence) |
Oral |
- Take with food
- Approved for use in treatment-experienced patients with NNRTI resistance
|
200 mg twice daily |
Nevirapine
Immediate release
(Viramune)
Nevirapine
Extended release
(Viramune XR) |
Oral |
- Increased risk of hepatic failure in women with CD4 counts >250 cells/mm3 and males with CD4 counts >400 cells/mm3
|
Immediate release
200 mg once daily for 2 weeks, and then 200 mg twice daily
Extended release
200 mg once daily for 2 weeks, and then 400 mg once daily |
Rilpivirine
(Edurant) |
Oral |
- Do not use in patients with baseline HIV viral load > 100,000 copies/mL or patients with baseline CD4 count <200 cells/mm3 due to increased risk for virologic failure
|
25 mg once daily with food |
| Source: References 12, 37-39 |
| Abbreviation: NNRTI, nonnucleoside reverse transcriptase inhibitor |
| Table 7. Integrase Inhibitors |
Generic Name
(Brand Name) |
Route of Administration |
Clinical Pearls |
Usual Adult Dosing |
Bictegravir
(Biktarvy*) |
Oral |
- Higher genetic barrier (to resistance) compared with elvitegravir and raltegravir
- Primarily metabolized through glucuronidation with few CYP450 drug interactions
|
50 mg once daily |
Dolutegravir
(Tivicay) |
Oral |
- Higher genetic barrier (to resistance) compared with elvitegravir and raltegravir
- Well tolerated, with insomnia and diarrhea being the most common adverse effects
- Primarily metabolized through glucuronidation with few CYP450 drug interactions
- Risk of neural tube defects should be taken into consideration when selecting for women of childbearing age
|
50 mg once daily |
Elvitegravir
(Genvoya**) |
Oral |
- Requires pharmacoenhancer
- Metabolized via CYP 3A4 enzymes and thus prone to drug-drug interactions
|
150 mg once daily with food |
Raltegravir
(Isentress) |
Oral |
- Adverse effects include insomnia, fatigue, and elevations in serum creatine kinase
- Primarily metabolized through glucuronidation with few CYP450 drug interactions
|
400 mg twice daily |
| Source: Reference 12 |
Abbreviations: CrCl, creatinine clearance; CYP and CYP450, cytochrome P-450; PI, protease inhibitor.
*Available only as a coformulated tablet with tenofovir alafenamide 25 mg and emtricitabine 200 mg.
**Available only as a coformulated tablet with cobicistat 150 mg, tenofovir alafenamide 10 mg, and emtricitabine 200 mg. |
| Table 8. Protease Inhibitors |
Generic Name
(Brand Name) |
Route of Administration |
Miscellaneous Information |
Usual Adult Dosing (with or without ritonavir/cobicistat) |
Atazanavir
(Reyataz) |
Oral |
- Take with food
- Hyperbilirubinemia
- Extensive clinical experience in pregnancy
- Endocrine disturbances*
|
With 100 mg ritonavir once daily
With 150 mg cobicistat once daily
300 mg once daily
Without ritonavir
400 mg once daily |
Darunavir
(Prezista) |
Oral |
- Take with food
- Good for PI-resistant virus
- Endocrine disturbances*
|
With 100 mg ritonavir once daily
With 150 mg cobicistat once daily
800 mg once daily
With 100 mg ritonavir twice daily
600 mg twice daily |
Fosamprenavir
(Lexiva) |
Oral |
- Not recommended as a first-line PI
- Endocrine disturbances*
|
With 100–200 mg ritonavir once daily
1400 mg once daily
With 100 mg ritonavir twice daily
700 mg twice daily
Without ritonavir
1400 mg twice daily |
Indinavir
(Crixivan) |
Oral |
- Not recommended as a first-line PI
- Nephrolithiasis
- Endocrine disturbances*
|
With 100–200 mg ritonavir twice daily
800 mg twice daily
Without ritonavir
800 mg every 8 hours |
Lopinavir/
ritonavir
(Kaletra) |
Oral |
- Extensive clinical experience in pregnancy
- Gastrointestinal intolerance
- Endocrine disturbances*
|
800/200 mg once daily
or
400/100 mg twice daily |
Nelfinavir
(Viracept) |
Oral |
- Take with meal
- Diarrhea
- Endocrine disturbances*
|
1250 mg twice daily
or
750 mg three times daily |
Ritonavir
(Norvir) |
Oral |
- Take with food
- Only used clinically as a pharmacoenhancer
- Endocrine disturbances*
|
Boosting dose
100 mg to 400 mg once to twice daily |
Saquinavir
(Invirase) |
Oral |
- QT prolongation
- Not recommended as a first line PI
- Endocrine disturbances*
|
With 100 mg ritonavir twice daily
1000 mg twice daily |
Tipranavir
(Aptivus) |
Oral |
- Intracranial hemorrhage
- Salvage PI
- Endocrine disturbances*
- FDA approved for use in treatment-experienced patients
|
With 200 mg ritonavir twice daily
500 mg twice daily |
| Source: Reference 12 |
Abbreviations: PI, protease inhibitor; FDA, Food and Drug Administration
*Endocrine disturbances include insulin resistance (type 2 diabetes), lipid abnormalities, peripheral fat loss, and central fat accumulation. |
| Table 9. Oral Antiretroviral Combination Products* |
| Generic Names (Brand Name) |
Usual Adult Dosing |
Emtricitabine, tenofovir disoproxil fumarate, efavirenz
(Atripla) |
1 tablet at bedtime on an empty stomach |
Abacavir, lamivudine
(Epzicom) |
1 tablet once daily |
Tenofovir disoproxil fumarate, lamivudine (Cimduo) |
1 tablet once daily |
Emtricitabine, tenofovir disoproxil fumarate
(Truvada) |
1 tablet once daily |
Emtricitabine, tenofovir alafenamide
(Descovy) |
1 tablet once daily |
Abacavir, lamivudine, zidovudine
(Trizivir) |
1 tablet twice daily |
Lamivudine, zidovudine
(Combivir) |
1 tablet twice daily |
Tenofovir disoproxil fumarate, rilpivirine, emtricitabine
(Complera) |
1 tablet once daily with food |
Tenofovir alafenamide, rilpivirine, emtricitabine
(Odefsey) |
1 tablet once daily with food |
Tenofovir disoproxil fumarate, lamivudine, doravirine
(Delstrigo) |
1 tablet once daily |
Tenofovir disoproxil fumarate, lamivudine, efavirenz
(Symfi, Symfi Lo) |
1 tablet once daily |
Tenofovir alafenamide, elvitegravir,emtricitabine,
cobicistat
(Genvoya) |
1 tablet once daily with food |
Tenofovir disoproxil fumarate, elvitegravir, emtricitabine, cobicistat
(Stribild) |
1 tablet once daily with food |
Dolutegravir, abacavir, lamivudine
(Triumeq) |
1 tablet once daily |
Bictegravir, tenofovir alafenamide, emtricitabine
(Biktarvy) |
1 tablet once daily |
Dolutegravir, rilpivirine
(Juluca) |
1 tablet once daily with food |
Darunavir, cobicistat, tenofovir alafenamide, emtricitabine
(Symtuza) |
1 tablet once daily with food |
Darunavir, cobicistat
(Prezcobix) |
1 tablet once daily with food |
Atazanavir, cobicistat
(Evotaz) |
1 tablet once daily with food |
Source: Reference 12.
For Clinical Pearls relevant to these oral combination products, see individual agents listed in Tables 4–8. |
Treatment-experienced patients can be more challenging than treatment-naive patients because therapeutic strategy is often driven by genotypic resistance/mutations, medication adherence, and previous exposure to other agents.12 Common genetic mutations include M184V and K103N. The M184V mutation confers a high level of resistance to lamivudine and emtricitabine while K103N produces high levels of resistance to efavirenz and nevirapine.12 As a result, genotypic, phenotypic, and co-receptor tropism assays are recommended to be used to assess viral strains and guide the selection of antiretroviral drug regimens.12 Genotypic assays test for the presence of mutations known to confer viral resistance. Phenotypic assays (typically reserved for complex patterns of resistance) test for the antiretroviral inhibitory concentration required to decrease HIV replication by 50%. Co-receptor tropism assays are recommended when the CCR5 antagonist, maraviroc, is being considered or if virologic failure occurs during CCR5 antagonist therapy.12
Two drawbacks to resistance testing include: (1) testing is not beneficial in patients who have a plasma viral load that is less than 500 copies/mL, and (2) testing requires expert consultation. On the other hand, resistance testing has shown to be an independent predictor of virologic outcome and carries the potential to limit patient drug exposures and toxicities. HIV infection guidelines recommend resistance testing in the following circumstances12:
- At patient entrance into care
- In treatment-naive patients with chronic HIV infection
- In treatment-experienced patients who have shown complex-resistance patterns
- All pregnant women with HIV infection
- Virologic failure during antiretroviral therapy
- Suboptimal suppression of viral load after initiating antiretroviral therapy
- Before initiating antiretroviral therapy in acute HIV infection
Generally speaking, a new regimen for a treatment-experienced patient should include 2 or more antiretrovirals that are expected to have uncompromised activity on the basis of the patient’s treatment history and drug resistance test results. For example, protease inhibitors and dolutegravir have a high genetic barrier to resistance because multiple mutations are needed before resistance develops; they should be considered in nonadherent patients. Conversely, efavirenz and rilpivirine have low genetic barriers and may not be appropriate in this patient population.12 Notably, NRTI-sparing regimens have been used in both treatment-naive and treatment-experienced patients, although results have been mixed.41-43 Assessing and managing a patient who has experienced treatment failure is complex. As a result, expert consultation should be considered.
OPPORTUNISTIC INFECTIONS—PRIMARY PROPHYLAXIS AND VACCINES AS STANDARD OF CARE
Opportunistic infections (OIs) are pathognomonic in many new cases of HIV infection. The risk of acquiring particular OIs is based on the immune status of the patient. For instance, when CD4 cells decline to fewer than 200 cells/mm3, patients are at increased risk of acquiring Pneumocystis jirovecii pneumonia (PJP).13 Patients who are infected with PJP often present with multiple respiratory symptoms; hypoxemia and radiologic findings appear to be most suggestive of PJP. Patients with HIV should receive primary prophylaxis for PJP when their CD4 count is less than 200 cells/mm3, if the percentage of CD4 is less than 14%, or if oropharyngeal candidiasis is present. Prophylactic therapies include the following:
- Trimethoprim-sulfamethoxazole (TMP-SMX) 1 double-strength tablet orally once daily or 3 times weekly
- Dapsone 100 mg orally once daily
- Dapsone 50 mg orally once daily plus (pyrimethamine 50 mg and leucovorin 25 mg) once weekly
- Aerosolized pentamidine 300 mg administered once a month via the Respirgard II nebulizer
- Atovaquone 1500 mg orally once daily
Of the above-mentioned treatment options, TMP-SMX is considered preferred therapy. When a patient’s CD4 count increases to ≥200 cells/mm3 for at least 3 months in response to antiretroviral therapy, primary prophylaxis may be discontinued.13
When CD4 cells decline to fewer than 100 cells/mm3, patients are at increased risk of acquiring toxoplasmosis encephalitis, caused by the protozoan Toxoplasma gondii.13 Toxoplasmosis is almost exclusively a reactivation phenomenon, as most patients who develop the disease are seropositive for anti-toxoplasma immunoglobulin G (IgG) antibodies.13
Primary prophylaxis for toxoplasmosis should be initiated in patients with toxoplasma IgG whose CD4 counts are below 100 cells/mm3. The drug regimen of choice is TMP-SMX 1 double-strength tablet daily. For patients seropositive for Toxoplasma gondii who cannot tolerate TMP-SMX, recommended alternatives for prophylaxis against toxoplasmosis include dapsone plus pyrimethamine plus leucovorin or atovaquone with or without pyrimethamine plus leucovorin.13 Primary prophylaxis for toxoplasmosis may be discontinued when a patient’s CD4 count increases to ≥200 cells/mm3 for at least 3 months in response to antiretroviral therapy.13
Unlike with PJP, patients may be able to take protective measures against the acquisition of toxoplasmosis because undercooked meats and cat litter have been identified as vectors of transmission. While TMP-SMX is an appropriate prophylactic regimen for toxoplasmosis, it should not be used to treat patients with active disease. Patients with active disease should be treated with a 3-drug combination that consists of sulfadiazine plus pyrimethamine plus leucovorin for at least 6 weeks.13
Moreover, when CD4 cells decline to fewer than 50 cells/mm3 patients may also be at increased risk for mycobacterial infections, in particular Mycobacterium avium complex (MAC). However, primary prophylaxis should not be initiated until the CD4 cell count falls to fewer than 50 cells/mm3and disseminated infection has been ruled out. Aside from impaired immune function, other factors may also contribute to active disease such as high viral load, previous opportunistic infection(s), and colonization with MAC in the respiratory or gastrointestinal tract. In patients who are antiretroviral therapy (ART)–naive, active disease can mimic tuberculosis symptoms including night sweats, fever, and weight loss. The prophylactic agents of choice are the macrolides — azithromycin and clarithromycin. If a patient is unable to tolerate either agent, rifabutin is an option; however, rifabutin has many drug-drug interactions that complicate its use with antiretrovirals. Primary prophylaxis for MAC may be discontinued when a patient’s CD4 count increases to ≥100 cells/mm3 for at least 3 months in response to antiretroviral therapy. It should also be noted that MAC prophylaxis should be reintroduced if the CD4 count returns to below 50 cells/mm3.
For patients who require therapy for active infection, clarithromycin plus ethambutol is recommended for initial therapy, and some experts add rifabutin to the initial regimen. In certain scenarios, such as lack of ART with concurrent infection, a third or fourth drug should be considered such as a fluoroquinolone or aminoglycoside. Therapy usually must be instituted for a minimum of 12 months in conjunction with restored immune function (CD4 count >100 cells/mm3 for >6 months) and absence of signs of MAC infection.13
Globally, tuberculosis remains a common coinfection with HIV. Patients with latent tuberculosis infection (LTBI) are at significantly higher risk of reactivation compared with patients who do not have HIV infection. Patients with both LTBI and HIV infection should receive isoniazid 300 mg orally once daily plus pyridoxine 25 mg orally once daily for 9 months.13 However, before prophylactic treatment is started, active tuberculosis must be excluded by a negative chest radiograph and the absence of symptoms. Alternative LTBI drug regimens include rifampin 600 mg orally once daily for 4 months or rifabutin (dose adjusted for concomitant antiretroviral therapy) for 4 months. Rifabutin is a less potent CYP3A4 inducer than rifampin and is preferred in patients receiving protease inhibitors. It is important to note that once-weekly isoniazid plus rifapentine is not recommended for LTBI-HIV coinfection because rifapentine can result in development of rifamycin resistance in patients living with HIV.13 For patients with active tuberculosis, there has been much controversy regarding when to initiate treatment. The Starting ART at 3 Points in TB (SAPIT) and Cambodian Early versus Late Introduction of Antiretroviral Drugs (CAMELIA) trials showed that earlier therapy was associated with a mortality benefit.44,45
In addition to prophylaxis of select OIs, vaccines are an important preventive measure in patients who are immunocompromised. Table 10 lists CDC-recommended vaccinations for patients with HIV infection.46 Notably, 13-valent pneumococcal conjugate vaccine (PCV13) has recently been recommended for use in adults with HIV infection. Specifically, all patients with HIV infection who have never received pneumococcal vaccine should receive a single dose of PCV13, followed by a dose of 23-valent pneumococcal polysaccharide vaccine (PPSV23) no earlier than 8 weeks later.13 However, it may be preferable to wait until a patient’s CD4 count increases to >200 cells/mm3 before initiating PPSV23.13 Live vaccines should generally be avoided in patients with HIV infection, especially those with CD4 counts <200 cells/mm3.
| Table 10. Recommended Immunizations for Adult Patients with HIV Infection by CD4 Count* |
| Vaccines |
CD4 count <200 cells/mm3 |
CD4 count ≥200 cells/mm3 |
| Influenza |
Recommended annually (inactivated influenza vaccine only) |
| Td/Tdap |
1 dose of Tdap followed by Td booster every 10 years |
| Shingles |
Not recommended |
| PCV13 |
1 dose |
| PPSV23 |
1 to 2 doses |
| Meningococcal |
1 or more doses |
| MMR |
Not recommended |
1 or 2 doses |
| HPV for women |
3 doses through age 26 years** |
| HPV for men |
3 doses through age 26 years** |
| Varicella |
Not recommended |
2 doses |
| Hepatitis A |
2 doses |
| Hepatitis B |
3 doses |
| Hib |
1 or 3 doses |
Abbreviations: Td, Tetanus diphtheria; Tdap, Tetanus-diphtheria-pertussis; PCV13, 13-valent pneumococcal conjugate vaccine; PPSV23, 23-valent pneumococcal polysaccharide vaccine; MMR, measles-mumps-rubella; HPV, human papillomavirus; Hib, Haemophilus influenzae type b.
| Generally recommended vaccines. |
| These vaccines are not recommended based on CD4 counts and other factors. |
| These vaccine schedules may be recommended based on an individual's lifestyle. |
*Data derived from Centers for Disease Control and Prevention46
**At the time this program was prepared, the Food and Drug Administration had expanded the age indication for the 9-valent HPV vaccine product Gardasil 9 to include men and women through age 45 years, but the Centers for Disease Control and Prevention had not changed its recommendations on this earlier age. |
FLORIDA LAW RELATED TO HIV/AIDS TESTING
In 1988, Florida became one of the first states to adopt comprehensive legislature to manage the HIV/AIDS epidemic, which became known as the Florida Omnibus AIDS Act. Besides mandating specific continuing education requirements for health care professionals in Florida, the Act requires health care workers who order HIV tests to47:
- Obtain informed consent from the patient
- Confirm positive preliminary test results through subsequent tests before informing the patient of the result
- Take all reasonable efforts to notify the test subject about the test results
- Adhere to special handling requirements of superconfidential HIV test results
- Follow correct procedures when notifying parties other than the patient of HIV test results
- Report positive HIV test results to the local county health departments
Informed consent
According to Florida law, a patient must understand and agree to HIV testing, which means the patient, not the health care provider, determines if testing may occur.47 Importantly, when obtaining informed consent, which does not necessarily have to be in writing, the health care provider must take into consideration the age, mental capacity, and language skills of the patient. In addition, health care providers must explain the following information that pertains to testing47: (1) any information identifying the patient and the results of the test are confidential and protected against further disclosure; (2) individuals who test positive will be reported to the local county health department; (3) anonymous testing is available but the provider must inform the patient regarding the locations of alternate testing sites. Notably, minors in the state of Florida (children under the age of 18) are considered adults for the purposes of consenting to examination and treatment of STDs, including HIV testing and treatment. Florida specifically prohibits telling a minor’s parents about the examination or treatment for an STD, including HIV infection.47
Health care providers who perform HIV testing without patient informed consent are subject to discipline by their licensing bodies, including fines and license suspension or revocation. However, Florida law recognizes several circumstances that release health care providers from obtaining informed consent, including the following47:
- Pregnancy: Pregnant women must be advised that the health care provider attending to them will conduct an HIV test; however, the patient has the right to refuse, which is required to be in writing and must be placed in the patient’s medical record.
- Emergencies: A provider may test without consent in a “bona fide” medical emergency, provided documentation is placed in the chart that testing is necessary to provide appropriate medical care.
- Therapeutic privilege: Informed consent may be bypassed if the medical provider documents in the medical record that informed consent would be detrimental to the health of a patient suffering from an acute illness and test results are necessary for diagnostic purposes and to help guide appropriate medical care.
- Sexually transmissible diseases: Florida laws permit HIV testing for sexually transmissible diseases in certain patient populations, such as convicted prostitutes, inmates prior to release, and select medical examiner cases, without consent.
- Criminal acts: Victims of criminal offenses that involve transmission of body fluids may require the person convicted of the offense to be tested for HIV infection.
- Organ donations: Certain provisions permit testing without consent in specific specialty areas, such as organ and tissue donations.
- Research: Established epidemiologic research methods that ensure patient anonymity are exempted from consent requirements.
- Abandoned infants: If a physician determines that an HIV test is medically indicated, but the infant's parent(s) or legal guardian cannot be located after reasonable attempts, the test may be performed without consent.
- Significant exposure: Under limited circumstances, the blood of a source of significant exposure to medical personnel may be obtained without consent.
- Repeat HIV testing: Renewed consents are not required when monitoring the clinical progress of a previously diagnosed HIV-positive patient or to monitor for possible conversion from a significant exposure.
- Judicial Authority: A court has the authority to order an HIV test without the individual's consent.
Notification responsibilities and confidentiality
HIV testing was traditionally performed using ELISA and Western blot tests, which required an extended period of time to generate results.48 However, the aforementioned rapid HIV tests produce results in as few as 20 minutes. Data show that rapid HIV tests substantially increase the number of individuals who get tested as well as the number of individuals who receive their results in a timely manner, expediting the delivery of patient counseling, education, and treatment services.49
Health care professionals who order HIV tests have an obligation to make all reasonable efforts to notify an individual of his or her result.47 If a preliminary HIV test result is positive, the Omnibus AIDS Act specifies that a separate confirmatory HIV test must be performed before the final result can be disclosed to a patient. Conversely, a negative preliminary test result is considered definitive and no further testing is required. The amount of information that is required to be disseminated to the patient depends on the result of the HIV test.47 For instance, if a patient has a negative test result, the Act does not specify the amount of information that must be communicated to the patient beyond discussing the importance of preventing transmission. Conversely, if an HIV test is positive, the patient must be counseled on the following47: (1) the availability of appropriate medical and support services; (2) the importance of notifying partners who may have been exposed; and (3) preventing the transmission of HIV. Importantly, health care providers who order such tests are required to report all positive HIV test results to the county health department.
While patient medical records are generally considered confidential under most state and federal laws, the Omnibus AIDS Act renders any information related to HIV testing of an identifiable person and the results of such testing superconfidential, which means health care professionals have additional obligations to protect these data.47 The Act specifically outlines situations in which HIV test results may be disclosed, including the following (the list is not all inclusive)47:
- To the test subject or his or her legal representative.
- Employees and agents of health care providers may discuss the HIV status of an individual among themselves if they need to know.
- Health care providers may share HIV test information with other providers for the purpose of diagnosis and treatment.
- Health care providers who are involved in the delivery or a newborn may note the mother's HIV test status in the medical record of the newborn.
- Medical examiners must report positive HIV test results to the Florida Department of Health.
- In select circumstances, health care providers are permitted to tell the sexual and needle-sharing partners of HIV-positive patients that they have been exposed to HIV.
- Adults responsible for a child who has been placed in foster care or adoption may be told the HIV status of the child, provided they are directly involved in the placement, care, or custody of the child.
- Appropriate authorities in situations related to child sexual abuse and neglect may be notified of the child’s HIV status.
- Hospital staff and health care workers who have had significant exposure to high-risk body fluids may be notified on a need-to-know basis.
The punishment for debasing the confidentiality laws of the Omnibus HIV Act can be quite severe, as it is a first-degree misdemeanor. Anyone who violates the Act is subject to up to 1 year of imprisonment. Further, a 1998 amendment to the Act made it a third-degree felony, which carries punishment of up to 5 years’ imprisonment for anyone who maliciously breaches the confidentiality of STD information. Last, the Florida Supreme Court held that anyone may be sued for negligence based on the violation of the Act’s duty of confidentiality.47
FUTURE DIRECTIONS AND CONCLUSION
Antiretroviral pharmacotherapy has improved dramatically over the past 20 years, and efforts to develop vaccines and a cure for HIV infection are ongoing. The recent introduction of several newer agents has shifted the paradigm to treatment simplification with an emphasis on tolerability and safety. The current drug pipeline includes innovative agents that seek to further simplify or make existing antiretroviral therapies safer as well as offer novel formulations. These drugs include a long-acting injectable integrase inhibitor (cabotegravir), a vaginal ring containing active drug (dapivirine), and an attachment inhibitor (fostemsavir).50-52
Initiation of antiretroviral therapy is more important today than ever because of the direct patient and public health benefits. With the development of novel agents, continued access to care, and government funding, many of the existing challenges health care practitioners face today could be concerns of the past.
REFERENCES
- Peters PJ, Pontones P, Hoover KW, et al. HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N Engl J Med 2016; 375: 229–39.
- Joint United Nations Programme on HIV/AIDS (UNAIDS). Global HIV & AIDS Statistics – 2018 fact sheet. http://www.unaids.org/en/resources/fact-sheet. Accessed October 14, 2018.
- Maartens G, Celum C, Lewin S. HIV infection: epidemiology, pathogenesis, treatment, and prevention. 2014; 384:258-71.
- HIV incidence and prevalence in the United States, 2010-2015. HIV Surveillance Supplemental Report 2018;23(1). Centers for Disease Control and Prevention website. https://www.cdc.gov/hiv/pdf/library/slidesets/cdc-hiv-surveillance-genepi-2016.pdf. Accessed October 12, 2018.
- Reif S, Whetten K. Southern HIV/AIDS Strategy Initiative (SASI) Update: The Continuing HIV Crisis in the US South. Durham, NC: Duke Center for Health Policy and Inequalities Research; 2012. https://southernaids.files.wordpress.com/2012/11/sasi-update-the-continuing-hiv-crisis-in-the-us-south.pdf. Accessed October 12, 2018.
- Hurt CB, Dennis AM. Putting it all together: lessons from the Jackson HIV outbreak investigation. Sex Transm Dis. 2013;40(3):213-215.
- Aral SO, Padian NS, Holmes KK. Advances in multilevel approaches to understanding the epidemiology and prevention of sexually transmitted infections and HIV: an overview. J Infect Dis. 2005;191(suppl 1):S1-S6.
- Joint United Nations Programme on HIV/AIDS (UNAIDS). 90-90-90 – an ambitious treatment target to help end the AIDS epidemic. http://www.unaids.org/en/resources/documents/2017/90-90-90. Accessed October 14, 2018.
- Nilsson J, Kinloch-de-Loes S, Granrath A, et al. Early immune activation in gut-associated and peripheral lymphoid tissue during acute HIV infection. 2007;21:565-574.
- Gray F, Scaravilli F, Everall I, et al. Neuropathology of early HIV-1 infection. Brain Pathol. 1996;6:1-15.
- Daar ES, Pilcher CD, Hecht FM. Clinical presentation and diagnosis of primary HIV-1 infection. Curr Opin HIV AIDS. 2008;3:10.
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services website. Updated on October 25, 2018. https://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescent-arv/0. Accessed October 28, 2018.
- Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Department of Health and Human Services website. https://aidsinfo.nih.gov/guidelines/html/4/adult-and-adolescent-opportunistic-infection/0. Accessed October 14, 2018.
- Updated Guidelines for Antiretroviral Postexposure Prophylaxis After Sexual, Injection Drug Use, or Other Nonoccupational Exposure to HIV— United States, 2016. Department of Health and Human Services website. https://stacks.cdc.gov/view/cdc/38856. Accessed October 14, 2018.
- Busch MP, Kleinman SH, Nemo GJ. Current and emerging infectious risks of blood transfusions. JAMA. 2003;289(8):959-962.
- HIV transmission. Centers for Disease Control and Prevention website. http://www.cdc.gov/hiv/basics/transmission.html. Accessed October 14, 2018.
- Joyce MP, Kuhar D, Brooks JT. Notes from the field: occupationally acquired HIV infection among health care workers—United States, 1985-2013. MMWRMorb Mortal Wkly Rep. 2015;63(53):1245-1246.
- Occupational HIV transmission and prevention among health care workers. Centers for Disease Control and Prevention website. http://www.cdc.gov/hiv/risk/other/occupational.html. Accessed October 14, 2018.
- Kuhar DT, Henderson DK, Struble KA. Updated US Public Health Service guidelines for the management of occupational exposures to human immunodeficiency virus and recommendations for postexposure prophylaxis. Infect Control Hosp Epidemiol. 2013;34(9):875-892.
- State HIV laws. Centers for Disease Control and Prevention website. http://www.cdc.gov/hiv/policies/law/states/index.html. Accessed October 14, 2018.
- Centers for Disease Control and Prevention. IDU/HIV Prevention: Syringe Disinfection for Injection Drug Users. http://www.cdc.gov/idu/facts/disinfection.pdf. Published July 2004. Accessed October 14, 2018.
- US Public Health Service. Pre-exposure Prophylaxis for the Prevention of HIV Infection in the United States—2017 Update: A Clinical Practice Guideline. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf Accessed October 14, 2018.
- Molina JM, Charreau I, Spire B, et al. Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: an observational cohort study. Lancet HIV. 2017;4(9): e402-e410.
- Paxton LA, Hope T, Jaffe HW. Pre-exposure prophylaxis for HIV infection: what if it works? Lancet 2007;370:89–93.
- Lehman DA, Baeten J, McCoy CO, et al. Risk of drug resistance among persons acquiring HIV within a randomized clinical trial of single or dual-agent pre-exposure prophylaxis. J Infect Dis. 2015;211(8):1211-1218.
- Mugwanya KK, Donnell D, Celum C, et al. Sexual behaviour of heterosexual men and women receiving antiretroviral pre-exposure prophylaxis for HIV prevention: a longitudinal analysis. Lancet Infect Dis. 2013;13(12):1021-1028.
- US Department of Health and Human Services, Health Resources and Services Administration. Guide for HIV/AIDS Clinical Care. Rockville, MD: US Department of Health and Human Services; 2014.
- Update: HIV prophylaxis following non-occupational exposure. New York State Department of Health AIDS Institute website. https://www.hivguidelines.org/pep-for-hiv-prevention/non-occupational/. Accessed October 14, 2018.
- Information regarding the Oraquick In-Home HIV Test. US Food and Drug Administration website. http://www.fda.gov/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/PremarketApprovalsPMAs/ucm311895.htm. Accessed October 14, 2018.
- Information regarding the Home Access HIV-1 Test System. US Food and Drug Administration website. http://www.fda.gov/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/PremarketApprovalsPMAs/ucm311903.htm. Accessed October 14, 2018.
- Branson B. The future of HIV testing. J Acquir Immune Defic Syndr 2010;55(suppl 2):S102-S105.
- First and foremost: choosing and using first-line antiretroviral therapy. Clinical Care Options website. http://www.clinicaloptions.com/HIV/Treatment%20Updates/First-line%20ART/First-line_ART_Slides.aspx. Accessed October 14, 2018.
- Lennox JL, Landovitz R, Ribaudo HJ, et al. Efficacy and tolerability of 3 nonnucleoside reverse transcriptase inhibitor–sparing antiretroviral regimens for treatment-naive volunteers infected with HIV-1: a randomized controlled equivalence trial. Ann Intern Med. 2014;161(7):461-471.
- Lundgren JD, Babiker AG, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med.2015;373(9):795-807.
- Cahn P, Andrade-Villanueva J, Arribas JR, et al. Dual therapy with lopinavir and ritonavir plus lamivudine versus triple therapy with lopinavir and ritonavir plus two nucleoside reverse transcriptase inhibitors in antiretroviral-therapy-naive adults with HIV-1 infection: 48 week results of the randomised, open label, non-inferiority GARDEL trial. Lancet Infect Dis. 2014;14(7):572-580.
- Sax P, Tierney C, Collier A, et al. Abacavir-lamivudine versus tenofovir-emtricitabine for initial HIV-1 infection. N Engl J Med. 2009;361(23):2230-2240.
- Mollan KR, Smurzynski M Eron J et al. Association between efavirenz as initial therapy for HIV-1 infection and increased risk for suicidal ideation or attempted or completed suicide: an analysis of trial data. Ann Intern Med. 2014;161(1):1-10.
- van Leth F, Andrews S, Grinsztejn B. The effect of baseline CD4 cell count and HIV-1 viral load on the efficacy and safety of nevirapine or efavirenz-based first-line HAART. AIDS. 2005;19(5):463.
- Molina J-M, Cahn P, Grinsztejn B, et al; for ECHO Study Group. Rilpivirine versus efavirenz with tenofovir and emtricitabine in treatment-naive adults infected with HIV-1 (ECHO): a phase 3 randomised double-blind active-controlled trial. Lancet. 2011;378(9787):238-246.
- Cohen CJ, Andrade-Villanueva J, Clotet B, et al; for THRIVE Study Group. Rilpivirine versus efavirenz with two background nucleoside or nucleotide reverse transcriptase inhibitors in treatment-naive adults infected with HIV (THRIVE): a phase 3, randomised, non-inferiority trial. Lancet. 2011;378(9787):229-237.
- Ocfemia MC, Kim D, Ziebell R, et al. Prevalence and trends of transmitted drug resistance-associated mutations by duration of infection among persons newly diagnosed with HIV-1 infection: 5 states and 3 municipalities, US, 2006–2009. In: Proceedings from the 19th Conference on Retroviruses and Opportunistic Infections; March 5-8, 2012. Seattle, WA. Abstract 730.
- Raffi F, Babiker AG, Richert L; for the NEAT001/ANRS143 Study Group. Ritonavir-boosted darunavir combined with raltegravir or tenofovir-emtricitabine in antiretroviral-naive adults infected with HIV-1: 96 week results from the NEAT001/ANRS143 randomised non-inferiority trial. Lancet. 2014;384(9958):1942-1951.
- Stellbrink HJ, Le Fevre E, Carr A. Once-daily maraviroc versus tenofovir/emtricitabine each combined with darunavir/ritonavir for initial HIV-1 treatment. AIDS. 2016(May 15);30(8):1229-1238.
- Abdool Karim SS, Naidoo K, Grobler A, et al. Timing of initiation of antiretroviral drugs during tuberculosis therapy. N Engl J Med. 2010;362(8):697-706.
- Havlir DV, Kendall MA, Ive P, et al. Timing of antiretroviral therapy for HIV-1 infection and tuberculosis. N Engl J Med. 2011;365(16):1482-1491.
- Centers for Disease Control and Prevention, US Department of Health and Human Services. 2015 Recommended Immunizations: By Health Condition. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2015. http://www.cdc.gov/vaccines/schedules/downloads/adult/adult-schedule-easy-read.pdf. Accessed October 14, 2018.
- Hartog JP. The Florida Omnibus AIDS Act: A Brief Legal Guide for Healthcare Professionals. Florida Department of Health, Division of Disease Control and Health Prevention, Bureau of Communicable Diseases, HIV/AIDS and Hepatitis Section; 2013. http://www.floridahealth.gov/diseases-and-conditions/aids/administration/_documents/Omnibus-booklet-update-2013.pdf. Accessed October 14, 2018.
- Notice to readers: approval of a new rapid test for HIV antibody. Centers for Disease Control and Prevention website. http://www.cdc.gov/MMWR/preview/mmwrhtml/mm5146a5.htm. Accessed October 14, 2018.
- Pottie K, Medu O, Welch V, et al. Effect of rapid HIV testing on HIV incidence and services in populations at high risk for HIV exposure: an equity-focused systematic review. BMJ Open. 2014;4(12):e006859. doi:10.1136/bmjopen-2014-006859.
- Margolis DA, Gonzalez-Garcia J, Stellbrink HJ, et al. Long-acting intramuscular cabotegravir and rilpivirine in adults with HIV-1 infection (LATTE-2): 96-week results of a randomised, open-label, phase 2b, non-inferiority trial. Lancet. 2017;390(10101):1499-1510.
- Kozal M, Aberg J, Pialoux G et al. Phase 3 study of fostemsavir in heavily treatment-experienced HIV-1-infected participants: day 8 and week 24 primary efficacy and safety results (BRIGHTE Study, formerly 205888/AI438-047) Presented to: EACS — 16th European AIDS Conference, Milan, Italy, October 25-27, 2017.
- Baeten JM, Palanee-Phillips T, Brown ER, Schwartz K, Soto-Torres LE, Govender V, et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N Engl J Med. 2016;375(22):2121–2132.
Back to Top